An estimated 12,000 people in the U.S. contracted HIV from transfusions between 1978 and 1984, leaving the public terrified. In reaction, the US passed a blanket ban on organ collection from HIV-positive donors in 1988.
But by the late 1990s, screening procedures for HIV had become accurate enough to eliminate this worry. At the same time, the advent of effective antiretroviral drugs meant that HIV-infected people could expect to live to a relatively old age—and also develop all the disorders that come with growing old. Instead of suffering from sarcomas and other AIDS-associated diseases, people began to see their HIV-positive friends dying from liver and kidney diseases, says Peter Stock, a transplant surgeon at the University of California, San Francisco (UCSF). “The transplant community was slower in recognizing it had become a chronic disease,” he says. The situation was exacerbated by the fact that no insurance agencies would cover organ transplants into HIV-infected individuals.
But the number of people waiting for organ donations was growing each year: by 2000, some 74,000 people in the U.S. were waiting for donors, according to the Organ Procurement and Transplantation Network (OPTN) in Washington, DC, which tracks transplantations and manages policies for the HHS. With such a long waiting list, the reasoning went, transplanting a healthy organ into someone with a fatal viral infection would be denying that organ to someone who could live a long life. Additionally, doctors worried that since these the immune systems of HIV-infected individuals were already compromised, further immunosuppression with drugs could be dangerous.
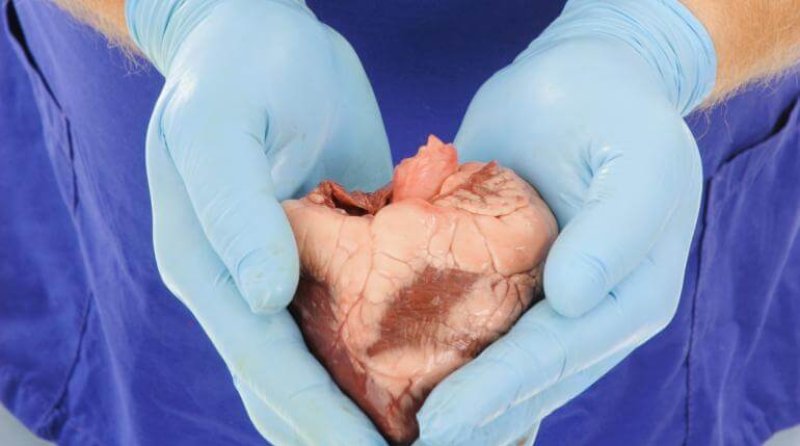
Stock wanted to at least explore the possibility that such transplants would succeed. In 1999, with the help of AIDS lobby groups and lesbian, gay, bisexual and transgender (LGBT) activists, he and his colleagues successfully lobbied the state of California to grant Stock’s team $3 million for a pilot study of transplanting uninfected livers and kidneys into HIV-positive recipients. The 37 patients from this study and a subsequent one appeared to do well overall and were only slightly more likely to reject organs than HIV-negative recipients were. But the grassroots effort provided enough preliminary evidence for Stock to receive a $25 million grant from the U.S. National Institute of Allergy and Infectious Diseases (NIAID) in 2003 to transplant livers and kidneys into 275 HIV-positive patients.
Read full, original article: Hopeful act: A rebel transplants organs from HIV-positive donors