Paxlovid, the most widely prescribed drug to treat symptomatic COVID-19, has lately attracted a number of detractors. News organizations have recently reported, for example, that it has “failed” in several clinical trials, including a recent one in which supposedly it didn’t improve symptoms in certain patients with COVID-19.

However, the nature of statistics in clinical trials is complicated and nonobvious, and in the case of Paxlovid, is worth a deep dive.
What works?
Paxlovid has been shown to be remarkably effective since its approval by the FDA under an Emergency Use Authorization for infected patients who are at high risk for serious outcomes such as hospitalization and death. What is commonly ignored, however, is that the expansive definition of “high risk” includes dozens of conditions in addition to those, like obesity, cancer, and immunosuppression, that are widely known.
Taken together, this list includes a very large segment of the U.S. population for whom the CDC says there is evidence of efficacy of Paxlovid on symptomatic COVID-19.
However, as Pfizer, the manufacturer of Paxlovid, expanded its clinical trials to “standard,” or lower-risk patient populations, the prevailing opinion was that the drug “failed” to work. But let’s examine the actual findings. . .
It’s true that the trial failed to meet its primary endpoint — a reduction in self-reported, sustained alleviation of all symptoms for four consecutive days. Although the results did not meet the requirements to attain formal statistical significance, Pfizer nonetheless reported that, “Data from standard-risk patients, both vaccinated and unvaccinated, while not all statistically significant, are supportive of efficacy data observed in [the] study.”
Additionally, a non-statistically significant 51% reduction was observed for the secondary endpoint of hospitalization or death in the Paxlovid-treated group. There were five incidents of hospitalization or death with drug treatment versus 10 with placebo (and 0 vs 1 death, respectively). Thus, the trends were in the right (effective) direction, but, given the small number of serious outcomes, it is not surprising that the data did not reach statistical significance.
There was also a “nominally significant” 62% drop in the prespecified secondary endpoint of COVID-19-related medical visits (emergency room, urgent care, etc.) per day in the drug-treated group compared with placebo in the full study population.
There were other favorable trends in parameters such as ICU admissions, but again, these did not achieve statistical significance. Thus, while the drug appeared to work, with many endpoints trending in the right direction, this trial could not satisfactorily prove it.
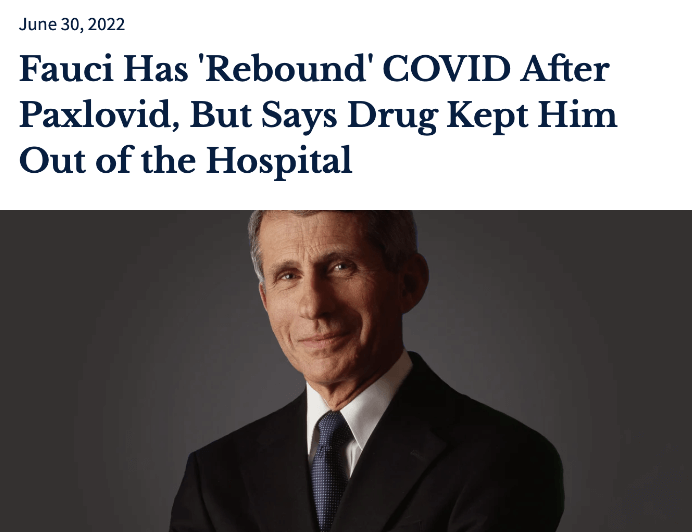
All of these factors contributed to Dr. Anthony Fauci’s renewed endorsement of the drug and even disclosing that he had suffered a “rebound” of COVID after taking the five-day course of the pills.
“Paxlovid did what it was supposed to do,” Dr. Fauci, told the New York Times in an interview, saying that he believed that he believes the treatment kept him out of the hospital and reduced the severity of his initial symptoms.
How to think of Paxlovid’s benefits
Rather than the drug “not working,” it’s more accurate to say that Paxlovid did not demonstrate efficacy in an “underpowered” trial – one with too few subjects to draw a valid conclusion. This is not uncommon when evaluating drugs; it occurs when the number of patients is not large enough and/or the difference in measured endpoints is small. For example, if we were to perform a clinical trial in the general population with a proven, licensed smallpox vaccine, the incidence of smallpox infection in both the vaccine-treated and placebo groups would be zero (because the disease is extinct), and we could not, therefore, conclude from the trial that the vaccine worked.
Pfizer was shooting for the stars with this trial in standard-risk patients. Because the drug works so well in preventing hospitalization and deaths in high-risk patients, it was not unreasonable to think it would successfully treat healthier people with milder infections. This may well be true, but the company has insufficient proof to get Paxlovid approved for this indication.
There is another obscure aspect of this conundrum. The FDA’s Paxlovid Fact Sheet lists a huge number of drugs, many commonly prescribed, that might be hazardous when administered with Paxlovid. Younger patients, who are more likely to have a lower (but not negligible) risk of COVID-19 progressing to serious disease, are also more likely to be eligible to take Paxlovid because they take fewer prescription drugs. By contrast, older patients who tend have a higher risk of serious COVID-19 disease are far more likely to need the drug, despite taking multiple prescription drugs that may be problematic.
Where does all this leave us? Different doctors have been using the drug very differently. Some call in the prescription as soon as a patient has symptoms and a positive test; others prescribe it only when they feel it is necessary for a bona fide high-risk patient. Some avoid Paxlovid if the patient is taking any of the drugs on the hazardous interaction list, while others are willing to discontinue or adjust the dosage of the listed drugs. But these are not easy calls.
Like so much about this pandemic, there are few easy answers.
Henry Miller, a physician and molecular biologist, is a senior fellow at the Pacific Research Institute. He was the founding director of the Office of Biotechnology at the FDA. Find Dr. Miller on Twitter @henryimiller
Josh Bloom, ACSH’s Director of Chemical and Pharmaceutical Science, earned his Ph. D.in organic chemistry at the University of Virginia, followed by postdoctoral training at the University of Pennsylvania. His career 20+ year first career was drug discovery research at Wyeth. (Disclosure: He has a small amount of Pfizer stock in his IRA.) Find Dr. Bloom on Twitter @JoshBloomACSH