
There are 3 key categories of genes that are involved in this: DNA repair enzymes, tumor suppressor genes, and oncogenes. Because cancer is such a broad bucket of diseases, things that can contribute to cancer develop are different for different cancers and also multifactorial. I discussed this in my cancer biology 101 piece.
It is far less common that a single insult to your body will be the *cause* of cancer than an accumulation of exposures that can impact your ability to repair cellular damage which can lead to cells growing uncontrollably.
Cancer development can be impacted by inherited and acquired gene mutations
Inherited mutations are DNA mutations that are present in every cell of a person’s body. These are called ‘germline mutations’ and they occur in sperm and/or egg cells, so are passed to a fetus during fertilization and conception. These inherited mutations are the mutations that result in cancers occurring among people at earlier ages, including in children.
Acquired mutations are DNA mutations that occur over the course of a person’s lifetime. Acquired mutations are not present in sperm or egg cells, and often are only found in certain cell types. These are not passed to children. 80% of DNA mutations that lead to cancer are acquired mutations. These mutations typically increase over the course of someone’s life, which is why most cancers appear later in life.
Risk factors for cancer include genetic and lifestyle influences
Rough estimates suggest that 30-50% of all cancers are preventable as they are linked to modifiable risk factors. It is also important to note that simply engaging in some of these behaviors does not guarantee you will develop cancer, and on the converse, having the most healthy lifestyle does not guarantee you won’t develop cancer. Many things are out of our control.
Have you heard things like “aspartame causes cancer” or “glyphosate causes cancer”, or “red meat causes cancer”?
Spoiler: these claims are wildly misinterpreted and usually false.
Unfortunately, the term carcinogenic is widely misused. Sometimes intentionally, sometimes not. Carcinogenic means that the exposure has the potential to cause cancer, not that it does under all circumstances. It also means something different depending on who is applying the term.
Claims circulating about risks of cancer are a result of the International Agency for Research on Cancer (IARC).
The IARC is often conflated with the entire World Health Organization (WHO), but in reality, it is a single working group of the WHO. The WHO has many different entities, subgroups, and departments within it.
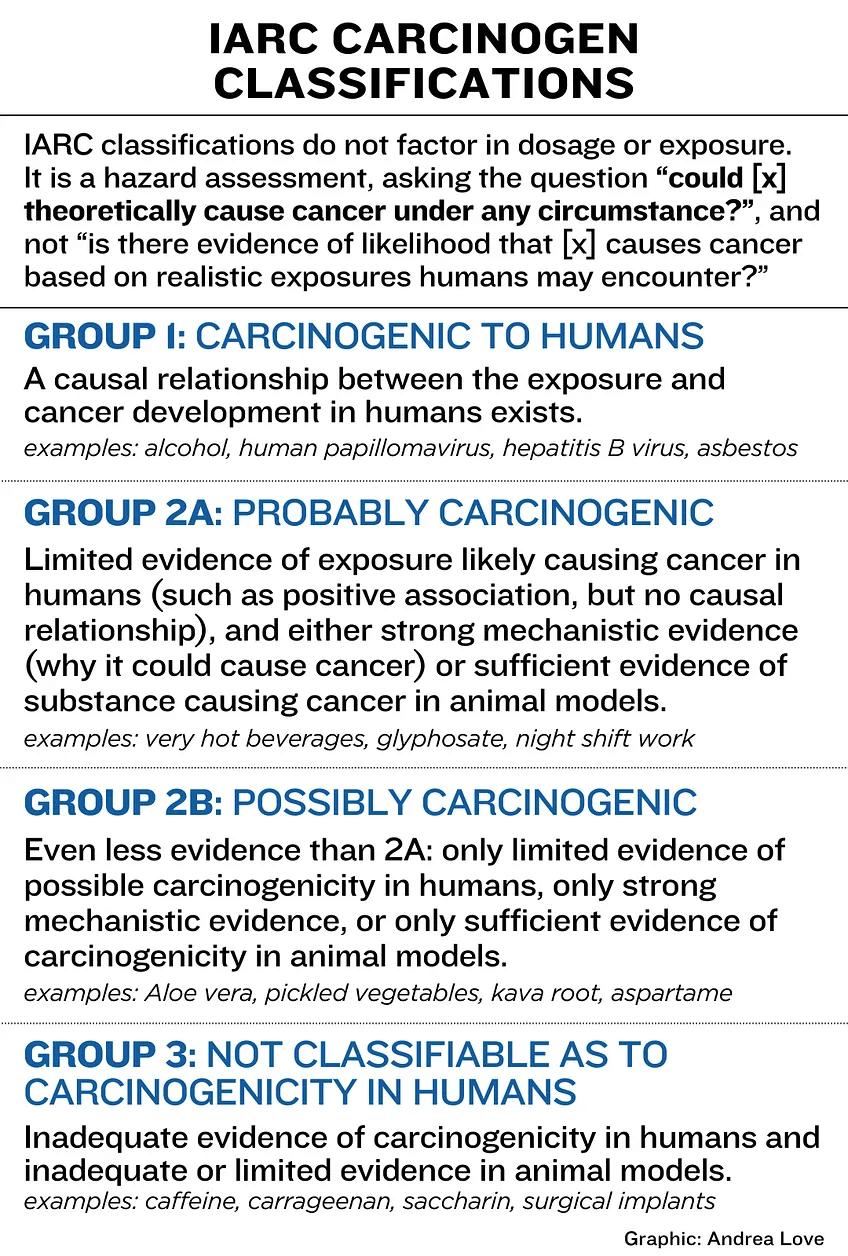
The IARC performs hazard assessments on exposures to assess for carcinogenicity and publishes monographs based on them. They do not conduct primary research. They also do not assess risk.
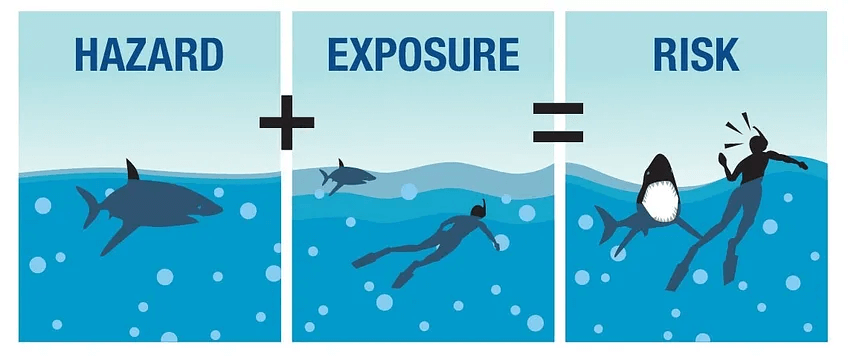
Hazard versus Risk: a key distinction that is often misunderstood
The IARC only identifies “cancer hazards” and not cancer risks.
Hazard refers to a hypothetical scenario in which, under any circumstance, even if unlikely, something bad can happen. In this case, the something bad would be cancer. Put another way, a cancer hazard is something that can potentially cause cancer.
Risk refers to the actual likelihood or possibility that something bad will happen if exposed to the hazard. Risk factors in both the hazard and the exposure. Put another way, a cancer risk is the probability that some exposure can cause cancer.
In the absence of a realistic exposure, a hazard does not present a risk.
The shark analogy is a great way to illustrate this.
If you’re standing on the beach, and the ocean has sharks swimming in it, a shark attack is a hazard. A shark attack can cause harm, but if you’re not in a scenario where you’d ever encounter it, there is no likelihood of that happening.
However, once you get into the water and start swimming, now you are in a situation where you might be exposed to the hazard, the shark attack. Now you have risk: the likelihood of a shark attack. This risk isn’t all or nothing either. The risk changes with where you are swimming, the types of sharks around, how long you’re in the water, how close you are to the sharks, how agitated they may be, etc.
The IARC carcinogenicity classifications are based on hazard, not risk.
When IARC submits their monographs, they are asking the question:
Could [x] theoretically cause cancer under any circumstance?
You can understand why so many exposures could be a “yes” there.
While the International Agency for Research on Cancer (IARC) plays a crucial role in evaluating the carcinogenicity of various substances, its classifications are often lacking important context. More than that, there have been a variety of recent instances where the IARC itself has cherry-picked data. Ultimately, this causes undue fear and confusion among the public, especially when an exposure in question relates to a common consumer product.
There are other issues with the IARC assessments:
Selective Use of Evidence: IARC often relies on selective interpretation of the available scientific evidence, sometimes over-emphasizing studies showing positive associations with cancer while disregarding more robust studies that show no such link. More than that, IARC routinely uses animal studies or in vitro studies during their assessments, and even among those, often only focuses on data that support their opinions, which is not what a scientific working group should do. Remember: you can do pretty much anything to cells in a Petri dish, but that doesn’t mean that it is representative of what is happening in a person.
Emphasis on Hazard, Not Risk: IARC focuses on assessing the hazard posed by a substance rather than the actual risk of exposure. This approach can lead to misleading conclusions, as it does not consider factors such as exposure levels and real-world usage patterns or realistic likelihoods of an exposure causing cancer.
Transparency issues: The methods and decision-making processes at IARC are not transparent. This lack of transparency has raised concerns about the objectivity and reliability of IARC’s classifications. IARC has been criticized by many scientific experts and other expert agencies, including those that have regulatory authority on exposures listed by IARC for lack of consistency and objectivity in their assessments. There have been several instances where robust human epidemiological evidence was excluded from IARC assessments when they did not demonstrate a link between the exposure and cancer.
Conflict of Interest: There have been allegations of conflicts of interest among IARC panel members, as some experts involved in the evaluations have been found to have ties to advocacy groups or industries with vested interests in the outcomes of the IARC assessments. For example, glyphosate was listed as class 2B as a result of the IARC excluding a decades-long study of 50,000 farm applicators that demonstrated no causal relationship between glyphosate and cancer, which undermines the safety of some conventional farming. IARC members have ties to organic farming industry members, which serve to benefit from the vilification of an herbicide used in conventional farming.
And I think, the biggest issue of all, which is really related to all the others:
Poor communication of findings: The IARC should be an impartial working group, but their activity over recent years suggests they are not. As a result, their findings are often not representative of what the body of evidence demonstrates. More than that, once their monographs are published, the IARC does not communicate to the public in a way that is nuanced and illustrative of the data. More often, the classifications are communicated in overly alarmist or sensationalized manners, leading to public confusion and misconceptions about the actual risks associated with certain exposures. Very few people even realize that IARC is based solely on hazard assessment to begin with, and reading headlines from media outlets that also don’t communicate that critical detail cause undue fear about substances that pose no realistic risk. This also exacerbates health anxiety, can lead to disordered eating, chronic stress, and more: all of which play a much greater impact on our health than many of the items included on the IARC lists.
What are some items IARC has classified?
IARC stratifies by group, with group 1 considered “carcinogenic”, group 2A “probably carcinogenic”, group 2B “possibly carcinogenic”, and group 3 “not classifiable.”
In this context, probably and possibly have very specific meanings. If you’re a parent, think about what you say if your kid asks you if they can have ice cream for breakfast. Do you sometimes say “maybe” to keep them from having a meltdown?
That’s what you can imagine probably and possibly to mean here. In that example, you know that maybe means no.
In group 1, there are some exposures that we do know are linked directly to cancers in humans, such as alcohol, asbestos, and several oncogenic viruses, like HPV. However, even with these items, the dose makes the poison (or cancer). It does not guarantee that these exposures cause cancer, only that there is a causal relationship between them.
However, from group 2A down, these items really have no causal evidence in humans. The criteria they use is very opaque, sometimes they cite animal studies only, sometimes in vitro studies, sometimes they only look at association or correlation, and ignore causally-linked data. You can see some of the things included: very hot beverages (above 149F or 65C), night shift work, pickled vegetables, aloe vera?
Every day I receive fear-driven messages from people who are terrified that the hot dog they ate, the diet soda they drank, the conventional produce they buy is giving them and their families cancer. This is because of poor messaging by IARC, inconsistent criteria that clearly is influenced by personal beliefs, and intentional manipulation of these classifications by social media influencers and activist groups who are determined to spread falsehoods and fear.
Based on that, I might argue that the IARC classification system, in our current era of disinformation, is doing more harm than good.
What do we actually need? Nuanced and measured plain language summaries that are based on risk assessments
The wellness industry is booming because people are riddled with health anxiety. Clickbait headlines saying hot dogs are causing cancer and cancer rates are rising at astronomical speed are not helping. More than that, they are not accurate.
Our scientific agencies and science communication should be committed to providing balanced information, not fanning the flames of misinformation. As someone who works in cancer immunology, I have been disappointed in the IARC for many years because of their lack of commitment to true evidence-based data review.
There are other agencies who do perform risk assessments on substances, and those are triaged by type of exposure. For example, the Joint FAO/WHO Expert Committee on Food Additives (JEFCA) assesses risk of harms of food additives, including non-nutritive sweeteners, preservatives, food colorings, etc. The European Food Safety Authority (EFSA) does the same. The European Chemicals Agency does this for chemicals, particularly pesticides. The problem is, these findings are almost always in conflict with the IARC findings because they are assessing actual risk, not hazard, and that confuses the public even more.
How should they know what to believe, especially when anti-science activists seize upon one headline and ignore the others?
That is why everyone should shift to a consistent method of safety assessment, or at least clearly define what approach is being used. Without this context, the public is going to be at the mercy of the misinformation of the day. And that is one of the biggest harms to public health, science literacy, and technological advancement today.
Dr. Andrea Love has a PhD in Immunology and Microbiology. Andrea is a subject-matter expert in infectious disease immunology, cancer immunology, and autoimmunity and is adept at translating complex scientific data and topics for the public and healthcare providers. Follow Andrea on X @dr_andrealove































