Using biology to determine the racial ancestry of human remains is racist. Except when it’s done in the name of anti-racism.
We urge all forensic anthropologists to abolish the practice of ancestry estimation.
Biological ancestry, moreover, plays no role in susceptibility to disease. Except when it does.
Despite social scientific perspectives that endorse a nonbiological basis to race, within biomedicine, biological uses of race remain entrenched due to their utility for identifying the causes of the disease.
Artificial intelligence (AI) systems identifying ‘race’ from medical images perpetuate systemic racism. Except when doing so ameliorates racial health disparities.
AI models can predict the demographics of patients, including race, directly from medical images, even though no distinguishing anatomical or physiological features are evident to human clinicians.
Above all, ‘race’ has no basis in biology. Except when it has.
Such contradictory conclusions can be drawn from an increasing number of studies of ‘race’, health and disease. The mixed messaging here is not merely contradictory and confusing; it potentially harms those from racial populations already bearing the brunt of health inequities, while also hindering efforts to close these often deadly divides.
Scientific racism?
To understand why, let’s begin with a standard example of this kind of research — a recent peer-reviewed academic study on apparent racial differences in plague deaths in 14th-century England. The analysis, based on skeletal remains from three medieval cemeteries in London, found “a significantly higher proportion of people of estimated African affiliation in the plague burials compared to the nonplague burials”. These findings were widely reported in the mainstream media (such as, in the UK, the left-leaning Guardian and the right-leaning Telegraph), with the BBC reporting the study under the headline, “Black women most likely to die in medieval plague”.

The study’s authors accept that these apparent racial differences in mortality might be an artifice of the small sample sizes (the remains of 145 individuals) used as the basis for the research. Nonetheless, their favored conclusion is that “these findings may reflect premodern structural racism’s devastating effects”. Of most relevance here, however, are two claims repeatedly emphasized throughout the researchers’ paper:
[1] the incorrect and harmful implication that there is a biological basis of race, and … [2] the incorrect inference that there is something inherent to people assigned to a certain racial category that makes them more vulnerable to disease
Racial identity and “decentering”
An obvious initial question, if (as the authors claim) race has no biological basis, is: how was an “estimated African affiliation” of centuries-old skeletal remains ascertained? The study acknowledges that racial affiliations were ultimately based on specific “macromorphoscopic traits” (features of the skull and facial bones) that differ between populations — in this case, “five traits with known heritability: anterior nasal spine, interorbital breadth, nasal aperture width, inferior nasal aperture, and nasal bone contour”.
Given that such traits are themselves the result of divergent biological evolution between geographically distinct ‘racial’ populations, this immediately raises another obvious question: does this not therefore reflect at least some underlying biological basis to race?
The researchers sidestep this issue. Instead, they argue that their analysis “includes data and tools that have been rightly critiqued for their role in perpetuating systemic racism, specifically the use of macromorphoscopic traits”. The authors — “keenly aware of the twinned whiteness of both anthropology and medieval studies” — suggest that to address this suspect historical aspect of their study, “whiteness must be decentered”. They “choose to foreground contexts and complexities, as well as white supremacist genealogies in forensic anthropology and medieval studies, as a form of methodological praxis as process”. In addition, to further “detach” the racial affiliation estimates from the racist “underpinnings of forensic anthropology,” the authors utilize cranial data that is “not attached to definitions of race and ethnicity”.
Although it is unclear what much of this rhetoric means, the authors appear to implicitly adhere to the widely-held ‘skin-deep’ concept of race. This view accepts superficial physical biological differences between racial groups but vehemently rejects the possibility of ‘deeper’ variation, such as cognitive or behavioral differences and in some cases even morphological differences. Such categorization, say many sociologists and cultural anthropologists, is what they call “scientific racism”.
While understandable as a reaction to historical and ongoing (albeit less prevalent) racist attitudes, denying any meaningful biological differences between racial populations can itself exacerbate existing racial disparities. This becomes clear when examining the other claim made above: that it is inherently wrong to assume that “people assigned to a certain racial category” may be more vulnerable to disease.
Disease susceptibility
While emphasizing that “race is a social classification and is not based in biological reality,” the study’s authors also state “that variation by race in susceptibility to and hazard of dying from disease reflects the biological and psychosocial effects of racism”. This seems to suggest a belief that increased vulnerability to a specific disease is the result solely of social behavior and prejudice.
Beyond a doubt, social factors — including racism — play a major role in health disparities between racial groups. But social environment is not solely the cause.
Equally beyond doubt, biological ancestry plays a crucial role in the prevalence and/or virulence of certain diseases in some populations and not others — the West African origins of sickle cell disease (an unfortunate by-product of increased evolved immunity to malaria) is a classic example, as are various hereditary genetic disorders (such Tay-Sachs and Gaucher disease) in Ashkenazi Jewish populations.
Other health disparities may be a combination of environmental factors, such as eating habits, and (biologically-mediated) genetic factors. Black Americans are 20% more likely to get colorectal cancer and die at a much higher rate, in part because, as a group, they consume greater amounts of animal fat than other ‘racial’ groups. Now researchers have identified gene mutations in cancer patients of African ancestry showing they are less likely to respond well to newer treatments.
The point is that simply blaming racism for all disparities in disease susceptibility and mortality may blind us to potentially crucial biological or genetic factors.
Exacerbating this issue is the insistence that race has no biological basis beyond, at most, superficial physical traits. This directly contradicts overwhelming evidence of meaningful genetic differences between racial groups (as discussed by GLP director Jon Entine and me with racial differences in the effects of Covid 19 and HIV/Aids). Ignoring this data, (as many scientists did even two years into the pandemic), risks derailing efforts to effectively tackle diseases that disproportionately affect marginalized communities.
For example, ‘biobanks’ (repositories of human genetic data) are already hugely skewed towards those of European ancestry. Take the UK Biobank, a biomedical database of “genetic, lifestyle and health information and biological samples from half a million UK participants”. While this is an invaluable resource for “the prevention, diagnosis, and treatment of a wide range of serious and life-threatening illnesses,” it only reflects the genetics of the British population as a whole — that is, overwhelmingly northern European. It is much less useful, however, in predicting health outcomes of those from other racial populations, whose genetic traits may differ across thousands of small genetic variations.
As psychologist Jonathan Anomaly points out, the lack of similar biobanks in, say, Africa or South Asia (that is, areas with poor health infrastructure and greater disease prevalence) means many of the most marginalized people in the world will be far less able than Europeans to “mitigate genetic risks through lifestyle changes and early medical interventions”. Further, Anomaly argues, that potential parents from other racial groups attempting in-vitro fertilization will also miss out on the choices increasingly available to prospective European parents.
Research taboos on ‘race’
In explaining this mismatch among different racial groups in the collection and use of useful genetic data, Anomaly points to “taboos surrounding research into genetic differences in socially significant traits” — that is, as highlighted above, the reluctance of many Western academics to accept that biology plays a part in racial variation and in differences in health outcomes.
Anomaly goes on to suggest, “Many social justice advocates say they want to help disadvantaged or poorly performing racial groups. But the taboos they’ve helped create in modern genetics research may end up depriving some ethnic groups of the opportunities that others will have.” (For his thoughtful analysis, Anomaly has been described as a “eugenicist” with “far right connections”.)
The plague study examined above also neatly illustrates another of Anomaly’s claims, that “the scientific establishment in Western liberal democracies has thoroughly absorbed the central dogma holding that race is an illusion, and that racial differences cannot exist”. Evidence of this is, for example, the “ethical guidance” by the editors of Nature Human Behaviour that unequivocally states: “Race and ethnicity are sociopolitical constructs. Humans do not have biological races, at least based on modern biological criteria for the identification of geographical races or subspecies.”
How, though, does this square with the “biological criteria’ (i.e., myriad genetic variations) that differentiate racial populations — biological differences that, moreover, have significant impacts on health outcomes?
Edging towards post-modernist nihilism
Fortunately, at least as yet, the scientific establishment has not embraced another feature of activist ‘scholarship’: a relativist approach to ‘truth’ (the idea that factual truth is relative to individuals’ cultural or social background). Consider the authors of the plague study, who claim their work aims to generate “multiple perspectives on truth … enabling a ‘pluralistic approach’ to a myriad of historical truths and methodological discoveries”. While historical events are often open to multiple interpretations, relativism extends and distorts this notion to imply that factual truth (like beauty) lies solely in the eye of the beholder — that ‘facts’ and ‘truth’ are determined by culture entirely. At an extreme, this fosters the insidious belief that science itself lacks objectivity and that so-called scientific ‘facts’ are nothing more than a reflection of Western colonialist biases.
However, by its own logic such relativism is incoherent and self-defeating; any claims made by relativist researchers are no more valid than any alternative ‘perspectives on truth’ that argue the opposite.
Interestingly, the relativist authors of the plague study demonstrate that they do accept some absolute truths — for example, in their claim that “the truth is that race (structural racism) was invented, refined, and rehearsed in medieval England”. The truth, it seems, is relative, except when it suits a specific ideological agenda. Consider the Sokal hoax.
The ‘post-modernist’ takeover of the social sciences began in the 1980s as a precursor to today’s social justice movement. It is marked by a general suspicion of reason and objectivity and an embrace of subjectivism and relativism. It was highlighted by the 1994 “Sokal hoax” in which a spoof academic article arguing that reality did not exist was published and lauded in a leading cultural studies journal.
Written deliberately as academic gibberish, his article, “Toward a Transformative Hermeneutics of Quantum Gravity, passed peer review with flying colors, and appeared in one of the notorious post-modernist journals of that era, Social Text. The article’s author, physicist Alan Sokal, later explained he wanted to draw attention to and therefore halt the “wanton abuse of science” by influential sections of the radical left. Unfortunately, in the intervening years, such “fashionable nonsense” has become more not less prevalent, and is now creeping deep into the hard science.
‘Race’, discrimination and AI
Before examining other questionable aspects of the plague study example, let’s briefly turn to an actual example of how supposedly ‘progressive’ ideological beliefs about race and racism can have a negative impact on real world scientific practice: recent advances and use of artificial intelligence (AI) technologies in medicine (technologies that, in theory at least, might do away with subjective human bias).
A slew of recent studies indicate that artificial intelligence models “are able to predict a patient’s self-reported race from their medical images” — and, moreover, can do so from images “that contain no indications of race detectable by human experts”.
In itself, this seems to undermine the claim that there is no biological basis to race. It’s what we make of this information that determines whether this information is racially harmful or not.
These reports on AI’s uncanny capacity to predict race are also replete with warnings of how this “can perpetuate racial bias in health care” and how it “mirrors unconscious thoughts, racism, and biases … [that] can lead to serious harm”. Likewise, it “raise[s] concerns about the possibility of AI systems to discriminate” and “introduces the potential for AI models to be biased and create racial disparities”. At an extreme, it could even “have catastrophic consequences by propagating deeply rooted societal biases”.
Concerns about how AI might exacerbate racial biases in medicine are not unfounded. Like any tool, artificial intelligence systems are susceptible to misuse and bias — as evidenced, for example, by algorithms that “used health costs as a proxy for health needs” only to falsely conclude “that Black patients are healthier than equally sick white patients, as less money was spent on them”.
But automatically equating this AI’s use or capabilities with societal prejudices (including racism) is misguided. The fact that AI can distinguish race from medical images is inherently neutral; the potential for harm lies not in any predictions themselves, but in how this information is interpreted. Bias and discrimination are not inevitable.
As the erroneous health costs paper also points out, one way to overcome AI’s potential for unintentional bias is through ‘open science’ — for instance, by ensuring relevant AI research and methodology is open for rigorous evaluation by all who use or are impacted by it. Another of the reports above similarly indicates how AI can be a “force for good” by instancing how “algorithms that learn from patients’ pain experiences can find new sources of knee pain in X-rays that disproportionately affect Black patients — and are disproportionately missed by radiologists”.
Again, such knee-jerk rejection of obvious biological aspects of race has the potential to further exacerbate existing unfair disparities. Indeed, fueling suspicions about inherent racism and prejudice within medical science creates a vicious circle by deterring non-white groups from participating in research. Lack of diverse data and over-representation of those with European ancestry — as with the genetic biobanks above — would then, in turn, impede greater appreciation of diseases with higher prevalence in specific non-white ancestry groups, ultimately harming patients who could benefit from targeted treatments.
Given that much of this potentially harmful obsession with racism comes from without the scientific community, medical researchers should perhaps take the following remedy for potential AI prejudice with a large grain of salt: “We need to bring social scientists into the picture.”
Progressive prejudice?
Human behaviorist Ian Leslie is scathing about the social scientists behind the plague victim study and the distorting influence that these kinds of ideas have on the academic discipline of history:
Whole fields of historical study seem to have turned into competitions for who can generate the most eye-catching narrative of identity-based injustice, and if that means making blatantly implausible empirical claims, so be it.
But here this distortion (in addition to the debilitating relativism critiqued above) extends further, into the wider scientific enterprise. As an example: the plague study authors emphasize that “Black Methodologies Matter”. While this may sound suitably progressive, it is a patronizingly racist claim that assumes all black researchers would follow and approve of the same methodologies. While scholars from traditionally underrepresented backgrounds can and do provide valuable insights into previously overlooked biases, framing research along racial or ethnic lines implies there are inherent, monolithic “white” or “black” (or “Asian” or “Native American” or a myriad other) methodologies.
It also segregates science, suggesting that black people are innately suited to studying black subjects, Asians Asian ones, whites white subjects and so on — the kind of thinking that would not have been out of place in apartheid South Africa.
The plague study authors take this one step further by stating their “hope to prioritize the methodologies of Black feminist archaeology”. Ignoring the implication that ‘feminism’ too is monolithic (it isn’t), where does this process stop? What about disabled, say, or transgender feminists from different ethnic groups — do they also have methodologies that must also be “prioritized” in scientific studies?
Ironically, highlighting ever-finer ‘intersections’ of identity simply reflects a standard right-wing trope on the absurdities of identity politics, that of a “disabled, black, lesbian woman” at “the top of a hierarchy of oppression”. The reality is that scientists and researchers are individuals, and the complex interplay of influences reflected in their work is not reducible to simplistic ‘identity’ labels.
Black feminist researchers can certainly bring valid perspectives to science, but the idea of “Black feminist methodologies” is ideological not scientific. Science is universal and cross-cultural, and it does not care about scientists’ identity. Rational, evidence-based scientific inquiry does not discriminate on the basis of who you are. All that matters is whether researchers’ methods and conclusions withstand scrutiny. While racist (or sexist or other prejudiced beliefs) have certainly influenced science — and scientific institutions have indeed followed discriminatory practices in the past — the hallmark of the scientific enterprise is that it is self-correcting.
Eventually, erroneous assumptions are found and weeded out through other scientists’ ongoing rigorous critiques. Thus, the claim that science is inherently ‘white’ or male is ludicrous; indeed, those who trumpet such beliefs perpetuate the prejudiced nonsense that science may be beyond the capabilities of those who are not white or Western or male — or, even more blatantly racist and sexist, that only white males can successfully practice science.
Potential dangers of anti-racist ideology
The study of plague victims exemplifies how anti-racist activism can harm those it purports to support. It also shows how researchers, research efforts and funding can be pushed toward currently fashionable causes rather than towards useful findings.
For instance, fourteenth-century England was a deeply stratified society and it has long been apparent that differences in socio-economic status lead to differences in health outcomes. Health disparities have persisted into the modern era, even as overall health and life spans increase — the rich (of whatever ‘race’) are still healthier and longer-lived than their poorer peers.
Studies of the effects of plague in historical and deeply unequal societies could, therefore, add to our understanding of both the impact and causes of disease on those at different social levels. The more we find out about how and why this occurs, the better able we will be to help those most affected by disease and ill health.
Compare this to the research critiqued above, a study that presupposes (on ideological grounds) that all health disparities are due solely to racism. This automatically precludes other, potentially more significant factors.
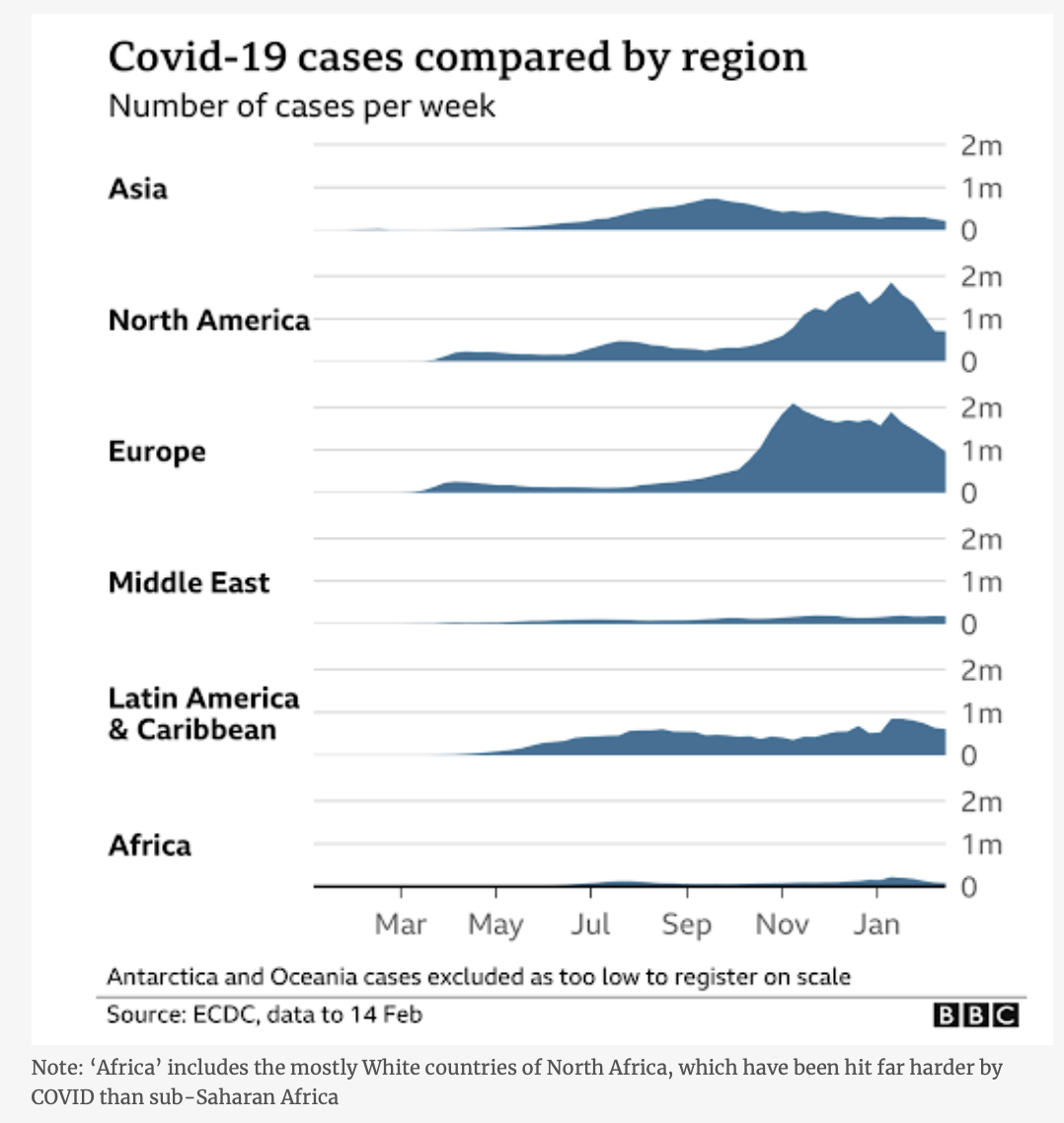
A recent example of the limitations of focusing solely on social determinants of health – discussed in greater detail in the Entine/Whittle article cited above – is the contrasting impact of COVID-19 on black people in the US (with disproportionately high mortality) and in Africa (where the impact seemed puzzlingly limited). Ignoring possible genetic factors limits our ability to fully understand the complex interactions between the environment (including racism and marginalization) and biology. This hinders our search for effective solutions.
Similarly, if we refuse to acknowledge any biological differences between racial populations, we will find it difficult to explain, let alone effectively address, the disproportionately high impact of HIV/Aids on black Africans compared to other racial groups. In short, racial identity could be a factor in why some people and not others suffer from disease.
Obsessing over racial categories while trumpeting questionable ideological beliefs does a disservice to science and, more importantly, to those from racial minority groups who currently gain least from advances in scientific and medical practice.
Patrick Whittle has a PhD in philosophy and is a freelance writer with a particular interest in the social and political implications of modern biological science. Follow him at patrickmichaelwhittle.com. Find Patrick on X @WhittlePM