It is important to temper somewhat the enthusiasm as this is but one case report. And it is only the beginning of use of engineered phage therapy as well as the first therapeutic use in a human mycobacterial infection.
To understand the stride, you must understand the patient.
This patient has Cystic Fibrosis (CF), an inherited disorder that is progressive and impacts multiple organ systems. Symptoms can occur along a spectrum, but this individual possesses among the most severe mutations and form. Put simply, the abnormal gene manifests by contributing to dysfunctional chloride channels in cells. Because this salt component (and its counterparts) can’t do what it is intended to do, a thick inspissated mucus accumulates in various organs thereby clogging airways and damaging the lungs while also facilitating many infections and other untoward effects.
This patient has the common CF problem of pancreatic insufficiency. This occurs when the mucus previously described infiltrates the pancreas leading to a spectrum of issues. Fat malabsorption due to diminished or impaired pancreatic enzyme production prompts malnutrition, fatty stools, and deficiencies in important fat-soluble vitamins. Patients can have a tough time keeping weight on which makes them less resilient to combat serious infections. Additionally, this patient has osteoporosis, liver disease and insulin-dependent diabetes. No doubt the medications necessary, like steroids, to treat underlying conditions and manage rejection avoidance of a bilateral lung transplant factor into the diabetes.
Patients in this realm of the spectrum are routinely on heavy duty antibiotics that warrant close surveillance of their kidney function, for example. They get rare bugs that even if treated effectively leave residual damage. It is what is done to the lungs over time that diminishes their capacity and, in the end, though there isn’t a cure for CF it is a lung transplant that can be essential for survival. Once obtained, then immunosuppressive drugs are required to tolerate the transplant. So, while solving the immediate breathing problem, a host of new issues can ensue.
This explanation barely scratches the surface, but gives a framework to understand the urgent need for medical advancement.
What needed to be done
Though we often hear of miraculous stories with respect to the successes of transplant, they are no walk in the park. The health and clinical status of the recipient at the time of transplant is crucial to the story. This patient was chronically infected with Pseudomonas aeruginosa (a common culprit in this population) and Mycobacterium abscessus subspecies massiliense taking anti-non-tuberculous mycobacteria treatment for the better part of a decade. The latter is known to contribute to significant post-transplant morbidity and mortality.
The bilateral lung transplant went well. But, after a week on immunosuppressive and many antibiotic medications, severe side effects necessitated stopping the intravenous (i.v.) antibiotics and maintaining the patient on i.v. nutrition. As redness at the surgical chest site expanded in and around the sternum, lung consolidations accrued as did skin and other lesions, and sputum grew M. abscessus, treatments were halted then resumed and so forth to control liver function derangements, destruction at the sternum and what was clearly a troublesome, life-threatening infection. To appreciate how severe the trajectory worsened it is critical to note the patient was not discharged until 7 months after transplant due to what was inevitably determined to be a disseminated mycobacterial infection (see below “source” section).
Ultimately, phage therapy was implemented which is what the authors ascribe to be associated with clinical improvement
“although we cannot exclude the possibility that patient gains would have occurred without phage treatment. However, we note that patients with similar clinical conditions typically have high morbidity and mortality, that improvement was not temporally associated with cessation or initiation of other drug administrations, and we show evidence to support in vivo phage replication. There were no adverse reactions to phage administration…”
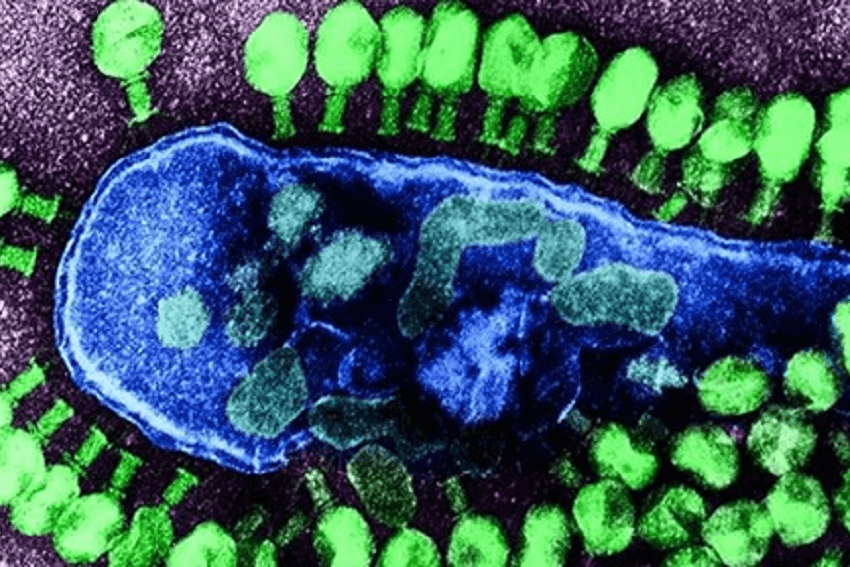
Bacteriophages (or “phages”) are viruses that can enter bacterial cells and use the resources of the host to do what is so desired in “phage therapy,” infect and kill it. This team had to use genome engineering and a triple cocktail of phages to achieve beyond the infecting bacteria portion and attain the kill part. Since phage therapy had not been used in this scenario before, there was a chance it could have a bad effect with the concern being in the immune system. Fortunately, this did not happen.
In the end
A three-phage cocktail was genetically engineered to manufacture “effective lytic derivatives that efficiently kill the infectious M. abscessus strain.” The patient, now a 17-year-old, is doing well. She is not cured, but is performing all of her regular activities, is fully at school and is still receiving therapies.
When antibiotic resistance in an extremely sick patient renders limited treatments, it is nice to know phage therapies could be an option. Though this solitary case is not a slam dunk for all circumstances, cautious optimism is reasonable as the field will only continue to be more and more researched, refined and, hopefully, perfected in humans so as the concerning potential effects can be avoided.
The source listed below details the process and methods utilized to engineer this treatment and reflects the origin of quotes used in this piece. This NPR link further investigates and elucidates how dire the situation was for this young woman by interviewing her and the family as well as the treating team.
Dr. Jamie Wells, MD, FAAP, is an award-winning board-certified physician with over a decade of experience caring for patients and the director of medicine at the American Council on Science and Health. Follow her on Twitter @jamiewellsmd
A version of this article was originally published on American Council on Science and Health’s website as “Genetically Engineered Phage Therapy ‘Saves’ Teen From Drug-Resistant Infection” and has been republished here with permission.































