Triple-negative breast cancer, about 10% of all breast cancers, is one of the most aggressive and deadliest forms of this terrible disease. One in 8 women in the United Sates and more than 2 million globally will be diagnosed with breast cancer in her lifetime with this particularly virulent form.
It’s called ‘triple-negative’ because the growth of the malignant cells are not promoted by estrogen, progesterone or the protein HER-2. More than 30,000 women in the US are diagnosed with it every year.
It’s more likely to attack younger women, under 50, and it disproportionately targets Blacks and those with the BRACA1 mutation. Even with advance treatment, only about three-quarters of victims survive.

But now there is new hope; remarkably a breast cancer vaccine might be in sight.
Shortly before last Christmas, the Food and Drug Administration (FDA) approved a breast cancer vaccine for clinical trials. The exact mechanism behind the increase in breast cancer rates is not yet fully understood but age, lifestyle choices and birth control interventions are all thought to increase risk. Although deaths from breast cancer have steadily gone down thanks to multiple breakthroughs in new therapies, a vaccine to prevent its development and progression could really swing the fight in favour of modern medicine.
Will vaccines against cancer become more common?
It is important with such a potentially breakthrough development to maintain a realistic perspective. If this vaccine passes all trials and gains approval for use in the clinic it will only be viable against 10-15% of all breast cancers and will likely have no effect on any other form of cancer.
It is unlikely that we will ever have a single vaccine or treatment that can cure every type of breast cancer or multiple forms of other cancers. That is wholly down to the vast array of biological differences that we observe between different cancer subtypes. Cancer cells mutate or switch different genes on/off depending on the tissue within which the cancer develops. In fact, cancers are so genetically and biologically variable that two patients can be diagnosed with the same type of cancer (lung for example) but present completely different genetic profiles in their tumour cells.
The idea that we could have a single drug or vaccine that could correct such a vast array of tumours is unrealistic, and this is evident in the highly specified approach to cancer research where the focus is on the development of highly specialised treatments.
How does a cancer vaccine work?
With that in mind then, how does a cancer vaccine like the triple-negative breast cancer jab actually work?
Generally, cancer vaccines can be divided into two categories based on how they attack the problem. The Anixa Biosciences vaccine is classified as a treatment vaccine and would be administered after diagnosis in an attempt to get rid of an already developed breast cancer. Treatment vaccines work by pitting the patient’s immune cells against the tumours that are invading their body. Cancer cells are foreign entities in our bodies and should be destroyed by our immune cells. They are, however, dangerously effective at evading our immune system and develop right under the nose of our vigilant immune cells by disguising themselves as “healthy cells”.
A treatment vaccine gives the cells of the immune system a small snippet of the ‘“foreign’” proteins that are present on the surface of a cancer cell to help it identify and destroy tumour cells. Treatment vaccines are very exciting tools in the fight against cancer and they can be specialized on a patient by patient basis but, as of yet, doctors have not been able to widely use them and they are often applied either in clinical trials or for use in specific circumstances. There is still difficulty in getting rid of larger tumors with a treatment vaccine and it is often difficult to stop the vaccine from triggering an all-out immune attack on a patients’ healthy cells. They are still a very viable option for future use but work clearly still needs to be done.
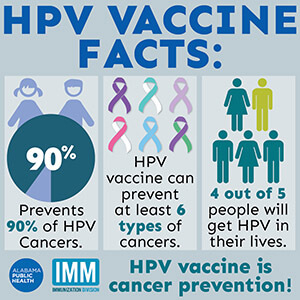
The second class of cancer vaccines are preventative vaccines. These are much more of a current success story. We have two fully approved preventive cancer vaccines, and many of you reading this may have already received your dose. Certain cancers can be triggered by viruses that remain in the body for too long. Cervical, vaginal and anal cancer can all be caused by the human papillomavirus (HPV); receiving a HPV vaccine has been shown to reduce incidence by nearly 90%.
Additionally, hepatitis B can cause liver cancer with 60-90% of hepatocellular carcinomas thought to be linked to chronic hepatitis B infection. Vaccinations against hepatitis B have, again, shown great promise with a study in Taiwan demonstrated that vaccinating infants reduced the incidence of liver cancer fourfold. Treatment vaccines are an exciting avenue for exploration, but we should not forget the principle that “prevention is better than cure” and preventative vaccines should remain as a significant part of our armory in the fight against cancer.
Multiple promising candidates
The Anixa Biosciences breast cancer vaccine is one of many being evaluated for clinical use as cancer vaccines continue to show promise. That same tactic of injecting patients with tumour cell proteins has shown promise in the treatment of melanoma; a serious and potentially fatal form of skin cancer. Researchers at the Harvard Medical School in Boston and the Broad Institute in Cambridge, Massachusetts have developed a personalised vaccine that trains immune cells to recognise proteins on the surface of melanoma cells and destroy them, leading to the complete removal of the cancer in 75% of the small group of participating patients.
Researchers are also now looking to take treatment vaccines a step further by injecting patients with whole cancer-cells to generate a faster and more specific response from the immune system. This is more than just a concept with the National Cancer Institute currently publishing the details of four ongoing clinical trials for the use of whole cell “allogeneic” to treat myeloma, pancreatic cancer and two breast cancer trials. The future definitely looks bright for cancer vaccines and your immune system is perhaps the best weapon you have against a disease like cancer.
How close are we?
The biggest question: how long until we see the regular use of vaccines to fight cancer? This is still a very complex issue and the efficacy of something like a cancer vaccine is limited by more than just the science. The scientific questions around what a cancer vaccine should target, how we limit damage to healthy cells and how effective they are at destroying the cancer still need to be answered by clinical trial data. Any therapy must pass multiple stages of rigorous clinical evaluation before it can be forwarded for approval. This certainly won’t happen overnight.
On top of that we have the issue of getting people to take a cancer vaccine in the first place. Take the HPV vaccine. The evidence that it prevents cervical cancer is overwhelming but the number of adult females getting the jab shot is low, and less than 11% of male candidates get the vaccine.
The last 12 months have highlighted the increase in public hesitation around taking any kind of vaccine. We must not forget about the importance of education and reassurance around the science involved if we want any cancer vaccine to be fully effective. It does not matter how good the product is if nobody feels safe taking it. You can have the best treatment in the world but if nobody wants to take it, what is it really worth?
Sam Moxon has a PhD in tissue engineering and is currently a research fellow in the field of regenerative medicine. He is a freelance writer with an interest in the development of new technologies to enhance medical therapies. Follow him on Twitter @DrSamMoxon
This article previously appeared on the GLP on March 16, 2021.