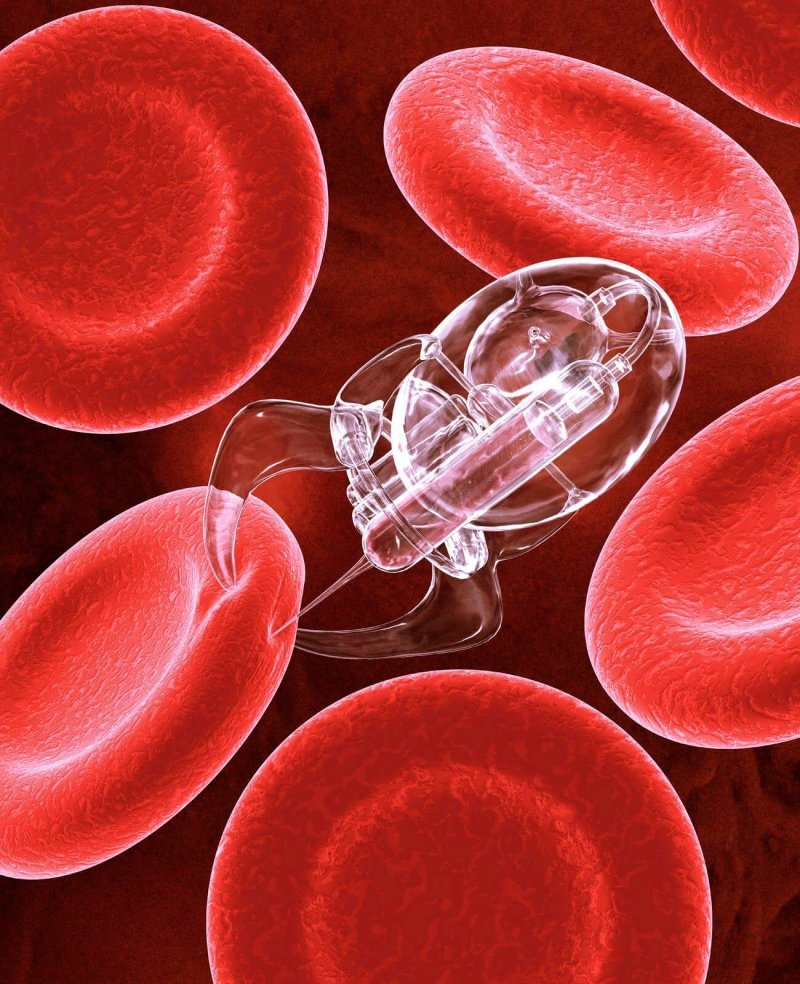
It’s been the stuff of science fiction for almost as long as there has been science fiction: Sending miniaturized machines or vehicles through the human body to go to sites of disease or damage and repair them internally, without the need for invasive surgical incisions and collateral tissue damage. Now the first version of one of these nanotechnologies has been realized in vivo (in a living body). Researchers at the University of California, San Diego have delivered microscopic treatment projectiles to the stomach of mice to explore the concept as a treatment for conditions such as stomach ulcers, gastritis, or other diseases of the organ.
Why it’s exciting
The concept of repairing wounds or treating disease internally has been of high interest to medicine likely from the use of the first poultices and treatments were administered to the ill and infirmed. Minimizing impact to surrounding tissues and eliminating the need for incision are two of the biggest draws to this technology – this limits the adjunct healing that needs to occur, thus presumably speeding recovery with less chance of over-correction. This is how many antibody-drug conjugates (ADC) currently work for approved therapies: a molecule-scale payload of chemotherapeutic or radiotherapeutic treatment is delivered directly to tumor sites or diseases cells by specific binding of the antibody component of the treatment; In this way only the diseased cells are targeted and damaged. This type of treatment in HER2-positive breast cancer, for example, leaves undiseased tissues undamaged by the therapy.
The future of this ‘payload-delivery’ therapy (PDT) is that each type could be specifically designed to affect a target disorder or disease, and therefore only impact that target. In much the same was as ADCs, but the PDT treatment could be developed to deploy at sites of (for example) ulcers, where the tissue could be healthy (and thus wouldn’t allow ADCs to attach) but in need of treatment.
The following transcript was part of Nobel laureate physicist Richard Feynman’s talk at the American Physical Society’s meeting at Caltech in December 1959, and captures the spirit of this branch of medical technology:
A friend of mine (Albert R. Hibbs) suggests a very interesting possibility for relatively small machines. He says that, although it is a very wild idea, it would be interesting in surgery if you could swallow the surgeon. You put the mechanical surgeon inside the blood vessel and it goes into the heart and “looks” around. (Of course the information has to be fed out.) It finds out which valve is the faulty one and takes a little knife and slices it out. Other small machines might be permanently incorporated in the body to assist some inadequately-functioning organ.
Drawbacks
Inducing immune response is used at times during treatments in order to increase the body’s healing response, and it’s likely that a treatment that’s done on too-small of a scale could in fact evade the body’s ability to detect and heal properly. Adjuvants are added to vaccines for the same reason: Adjuvants enhance the specific immune response to the vaccine antigens. It was observed in the 1920s that horses which developed abscesses at the site of diphtheria toxoid injections had higher antibody concentrations.
So to provoke a large enough healing response (in some instances) may require special treatment if it’s done by nanotechnological means. Will nanotechnology surgery produce the same sort of healing responses? The dogma is that leukocytes need to arrive at the injury site to prevent the infection by invading pathogens, but also to begin degrading and rebuilding tissue. However, we have been challenging this dogma and finding out many new strategies to potentially improve the speed and quality of wound healing by moderating the inflammation reactions.
Insight on the technology
This is an important in vivo step to moving this technology further ahead. It’s a step (mouse model) which needs to be taken in order to see if it even works, then human studies and safety trials can (and will) follow. As Richard Feynman observed about nanotechnology, as these technologies undoubtedly get more-and-more advanced (and perhaps more-and-more machine-like), there are several salient and critical principles to consider: Namely that devices and machines cannot be scaled down arbitrarily small (meaning we can’t just make things as small as we want): frictional forces, electrostatic forces, surface smoothness, and material strength become difficult properties to overcome. As Feynman observed (1959):
The metals that we use have a grain structure, and this would be very annoying at small scale because the material is not homogeneous. Plastics and glass and things of this amorphous nature are very much more homogeneous, and so we would have to make our machines out of such materials…
In addition, lubricants are ‘slippery’ only because many (many) molecules of the lubricant are allowed to pass around one another smoothly. When the gear that you’re trying to lubricate is getting shrunk-down to scales approaching the lubricant molecules themselves, they don’t act as lubricants anymore. The perceived viscosity increases rapidly as the machine parts get smaller and smaller.
The researchers have basically heeded Feynman’s statement in order to craft their PDT projectiles. How it’s intended to work is as follows: The ‘machines’ are really 20 micrometer-long conical polymer tubes coated in zinc. When they are exposed to stomach acid, the zinc reacts to generate hydrogen bubbles, which are forced out of the wider end of the tube, propelling it through the acid. Lead researcher on the invention, Wei Gao, observes, “Most previously reported self-propelled motors rely on non-biocompatible chemical fuels such as hydrogen peroxide.” The team’s projectiles are zinc-coated polymer, which is suitable for use in living animals. The group reports that the PDT projectiles can travel at about 60 micrometers (about 3 projectile-lengths) per second; they allege that this is fast enough to embed into the mucosal lining of the stomach.
There’s still a lot to work out before it’s ready for human trials or expectations of disease rectification; Right now the motion is basically random as the projectiles move around from different starting positions and orientations, and have small mean free paths (meaning that they are constantly bombarded and affected by the fluids and contents of the stomach), and whether this results in clinically-relevant improvement of conditions is a big set of open questions, but again it’s an important step forward in the progression of such technology.
Ben Locwin, PhD, MSc, MBA is a Contributor to the Genetic Literacy Project and is an author of a wide variety of scientific articles for books and magazines. He is also a researcher and consultant for a variety of industries including behavioral and psychological, aerospace, food and nutrition, pharmaceutical, petrochemical, and academic. Follow him at @BenLocwin.