It’s been a challenging few months for people with severe overweight issues mulling how best to shed what could be life-threatening pounds.
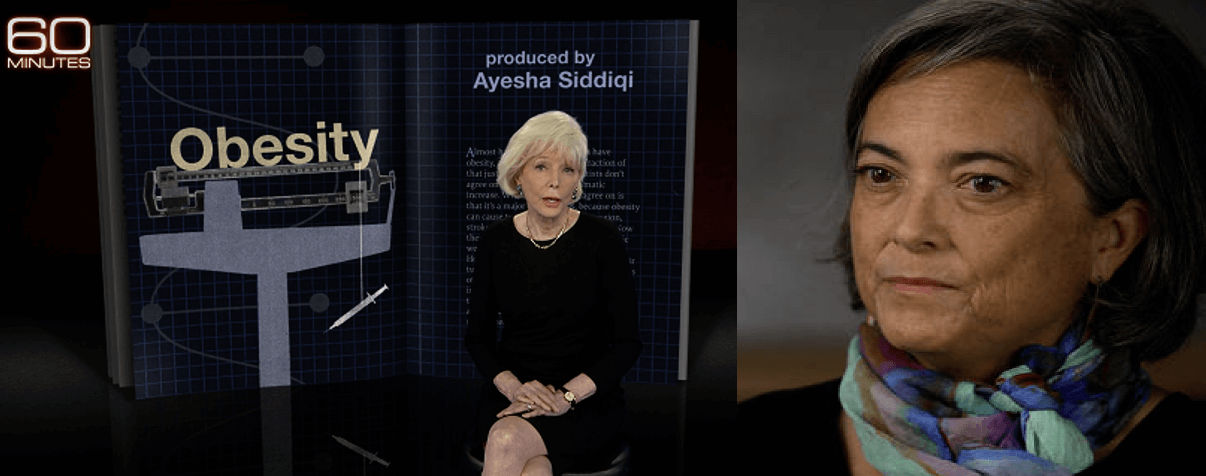
A debate over how to achieve that ignited when President Biden appointed Dr Fatima Cody Stanford, an obesity medicine physician at Mass General Health in Boston, to the 2025 Dietary Guidelines Advisory Committee. It blew up in intensity after her interview in January with Lesley Stahl on a 60 Minutes segment.
Dr. Stanford endorsed a growing consensus that genetics drives weight gain more the eating habits or lack of exercise.
The number one cause of obesity is genetics. That means that, if you were born to parents that have obesity, you have a 50 to 85% likelihood of having the disease yourself even with optimal diet, exercise, sleep management, stress management.
Those recommendations touched nerves. Critics and certain news outlets labeled her for appearing to dismiss the importance of exercise and good diet.
“Another delusional fantasist joins the Biden wrecking ball gang — what could possibly go right?”, said a New York Post reader. “The average commenter on NYP is more knowledgeable and has more common sense than these checked box hires will ever have,” said another.
Growing health concerns, growing treatment confusion
Obesity is a global health concern. About 2.8 million adults per year around the world die from being overweight or obese — the fifth highest risk of death globally. Being overweight or obese can carry increased risk of serious health complications like type 2 diabetes, heart disease and stroke. Recent studies suggest that being obese drastically increases the risk of developing dementia-causing illnesses like Alzheimer’s disease. One recent study demonstrated that body mass index (BMI) can be linked to brain health; young adults with a higher BMI showed a reduced ability to remember past events and older individuals with higher BMI exhibited brain shrinkage.
But figuring out root causes and designing effective treatment programs remains elusive. The science community, physicians, and nutritionists have flailed for years trying to come up with a consensus strategy.
According to Dr. Stanford, whose views could shape US policy for years, losing weight by changing eating or exercise patterns is a steep genetic hill to climb; lack of success, which in many cases is more likely than not, could feed into the hopelessness of patients who are limited in their ability to respond to behavioral changes. Genetic factors are key.
Dr. Shauna Levy, a bariatric surgery expert at Tulane University in New Orleans, worries about the message she’s standing. Dr. Levy emphasizes individual choice:
I think Dr Cody’s comment was an oversimplification of the cause of disease. However, I also think that as a society we likely underestimate the role of genetics in causing obesity and overestimate the role diet/exercise plays in treating this disease.
What we have here is the latest example of the age-old nature vs nurture debate — simplistic framing which tends to bring out the ideologue in people.
Multiple factors
It is easy to look at obesity as a problem with one primary variable: lifestyle. But the data suggest it’s far more complex than that, with genes the driving force. There are actually 50 genes strongly associated with obesity. This makes addressing the disease complex. It’s genetically multifactorial even beyond social factors.
The phrase ‘it’s not my fault, it’s genetic’ has become somewhat of a ‘meme’ in social discourse. That’s a misinterpretation of what Dr. Stanford said, but it’s the prism through which some people viewed her appointment.
In social discourse. Obesity is simple, many claim; it’s calories in versus calories out. Some critics have gone so far as to brandish the words of the CDC in an attempt to discredit the genetics perspective. They cite a line on the CDC website: “In most obese people, no single genetic cause can be identified”.
But that sentence is taken out of context. All it is saying is that simplistic belief that one gene can explain is not simplistic; almost no behavior or disease is caused by a single gene. Obesity, according to the CDC, can be caused by a combination of genetics and factors such as diet and exercise:
In most obese people, no single genetic cause can be identified. Since 2006, genome-wide association studies have found more than 50 genes associated with obesity, most with very small effects. Several of these genes also have variants that are associated with monogenic obesity, a phenomenon that has been observed in many other common conditions. Most obesity seems to be multifactorial, that is, the result of complex interactions among many genes and environmental factors.
Those who minimize the role of genetics worry its over-emphasis could leave obese people feeling hopeless, disincentivizing them to altering eating and exercise patterns. The fight against obesity, they say, could shift away from the whole person, an individual struggling with a disease. Their belief: Treatments can’t ‘short cut’ by looking at the symptoms of obesity and not the underlying causes.
New strategies such as using weight loss jabs that suppress appetite or drugs intended for use in patients with type II diabetes are controversial because of the potential for unintended and risky side effects. According to World Health Organization physician Dr. Nsisong Asanga:
Questions remain around the long-term impact of the medicine as a weight-loss tool. The most common side effects of the drug are nausea and diarrhea, but others listed include inflamed pancreas, vision changes, kidney failure, and allergic reactions, with the possible side effects still being observed.
What are the benefits that might justify the increased risk of using drug interventions? According to Asanga, that might depend on whether they patient becomes dependent on drug therapy.
Another study showed that once people stopped taking semaglutide, they gained all lost weight within a year – faster than they had lost it. They also lost any gains they made in heart or metabolism function. In other words, they only work for weight loss if you keep taking them.

Treating obesity is a complex challenge. Simple solutions in the form of a new pill or jab are not enough. Root causes need to be assessed and addressed.
Pediatricians stir more controversy
The American Academy of Pediatrics also inflamed the debate when it issued in January new guidance on treating childhood obesity. Their most controversial recommendation was an aggressive approach based on early intervention. AAP recommends offering obese children intense lifestyle treatments, coaching them in nutrition and physical activity. If that fails, the AAP suggests considering weight loss drugs and weight loss surgery, even for teenagers.
Critics who see the disease through a genetic lens say these strategies ignore the likelihood of a genetic component that could limit the success of lifestyle changes or drugs. Patients are made to feel terrible about themselves when lifestyle changes or drugs barely move the needled.
Critics also say it could result in pushing risky medications on children who are still growing into their bodies. But that’s a simplistic misreading of AAP recommendations. According to Dr. Edith Bracho-Sanchez, a pediatrician at New York-Presbyterian and Columbia University Irving Medical Center, they are quite layered.
They’re really offering a number of options, one of which is weight loss medication and surgery. But I think some of the coverage has focused on that out of context and the big picture has been missed.
Obesity is multifactorial. Nowhere is that more evident than in the content of the 50 genes so far linked to weight gain. Each of those genes affects the body in a unique way. Some genes make it physically harder for a person to lose weight while some could be “appetite genes” that make a person feel in a constant state of hunger, leading to overeating and obesity.
Add to the mix the link between childhood trauma and obesity: rewiring the brain to seek comfort in excess food consumption and it’s clear that an obese person with these genetic markers may not be “choosing” that lifestyle. Their desire to lose weight clashes with the biology of their body.
Genes are not destiny, however. Personal behavior often has a significant role in influencing the outcome of weight control problems regardless of genetic tendencies. The notion that ‘genes load the gun, but diet and lifestyle pull the trigger’ is pertinent. But there are some cases in which external environmental factors can make a person more likely to adopt a lifestyle that pulls that trigger.
Socioeconomic status, cultural background, mental health status and even occupation can influence the risk of obesity. Lecturing an overweight person to go for a run or eat more fruit or consume less processed food can be tone-deaf and unrealistic. Many of the people most impacted by obesity are poor. Some have occupations involving long hours of limited movement and many live in areas where healthier food comes at high a cost.
The causes and proposed ‘cures’ of obesity need to be contextualized. Genetics is a major contributing factor but should is not a ‘get out of jail free’ card to justify doing nothing. Casting a wider net of options provides medical professionals with more tools to treat obesity the way it should be addressed: on a case-by-case, personalized basis.
Sam Moxon has a PhD in tissue engineering and is currently a research fellow in the field of regenerative medicine. He is a freelance writer with an interest in the development of new technologies to enhance medical therapies. Follow him on Twitter @DrSamMoxon































