Did you get your flu shot this year? Did it work? Now is the time where the flu vaccine’s efficacy is formally measured by the Centers for Disease Control and Prevention (CDC) to determine how ‘good of a match’ the vaccine strains were compared with the circulating strains of influenza. I’ve heard this widely (and wildly) misinterpreted by everyone from the mainstream media to the general public to healthcare professionals.
This year’s vaccine efficacy? 50 percent.
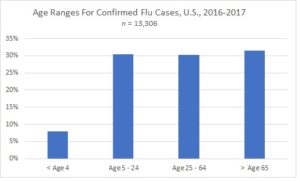
No, this does not mean the vaccine is half effective. It also doesn’t mean you have a coin flip’s chance of it helping you, and therefore you’re better off on your own. It’s actually a compound measurement taking into account 3,144 children and adults enrolled in the United States Influenza Vaccine Effectiveness Network, who were assessed between November 28, 2016 and February 4, 2017. The calculation involves two primary variables: the strain match by presenting cases that were laboratory confirmed flu illness, and the number of hospital visits avoided by vaccination. From October 2, 2016 through February 4, 2017, there were 38,244 positive tests for flu virus in the United States. Age was reported for 13,306 of those patients: 7.9 percent were younger than 5 years old; 30.4 percent were between 5 and 24 years old; 30.3 percent were between 25 and 64 years old; and 31.5 percent were 65 or older (see graphic below). There were more than 20 pediatric deaths reported this flu season as a result of the virus.
In a nutshell, the report is a good one: About half of those who otherwise would have been forced to seek professional care at a hospital didn’t have to because they were vaccinated. It’s much better than two years ago — when the vaccine was only 23 percent effective — and last year, when it hit 47 percent. The CDC measures this with a vaccine effectiveness (VE) point estimate. This season, the predominant viral strain is influenza A (specifically H3N2). The estimated vaccine effectiveness for H3N2 this season is about 43%. For influenza B, this season’s efficacy is about 73%. The overall protective effect is calculated to be about 48%. Interestingly, this effectiveness for H3N2 is quite good, because the strain tends to change more rapidly than influenza B or H1N1. The H3N2 strain was seen only on a limited basis last year, but this season’s strain is the same one that first appeared in the 2014-2015 flu season.
Let’s not forget that in 1918-19, the Spanish flu outbreak claimed 20 million to 50 million lives, while the 2009-10 pandemic saw only a tiny fraction of that, largely due to vaccination programs. But unfortunately, waiting for a problem does lead to behavior changes in the public — prior to the 2009-10 pandemic, hospital staff in the UK had flu vaccination rates of about 15 percent. During and following the pandemic season, vaccination rates surged above 50 percent.
Unlike other vaccines — for example, measles, mumps, rubella and tetanus — ‘seasonal’ influenza vaccines are still administered annually. That’s because antibody levels in the body drop after the flu season ends, usually after about 5 months. Additionally, each annual season brings a new set of predominant circulating strains, and so there is annual strain-matching performed to attempt to optimize the efficacy of each year’s vaccine with the strains likely to be circulating worldwide. The most promising avenues for a ‘one-time’ flu vaccine are based around using a highly-conserved viral protein that is found in all circulating flu viruses, and not relying on the rapidly-changing components that create the year-to-year differences.
Even with a non-exact match between the vaccine strain and a presenting strain, the vaccine can offer protection in the form of lessening the severity of the flu even if it is contracted. If we look at the arithmetic of this efficacy, we can see that a 50 percent reduction in flu hospitalizations for treatment times the number of doses administered in the U.S. ( approximately 150 million), yields about 74 million people not showing up at a clinic who potentially otherwise may have, and tens of billions of dollars in economic benefit due to avoidance of lost time, severe illness, medical treatment, and deaths. Oh, and by the way, this also means fewer people who are severely compromised and contagious with influenza walking around the general public — decreasing the chances of further spreading the flu to others, including perhaps you.
Ben Locwin, PhD, MBA, MS, is a contributor to the Genetic Literacy Project and is an author of a wide variety of scientific articles in books and magazines. He is an expert contact for the American Association of Pharmaceutical Scientists (AAPS), a committee member of the American Statistical Association (ASA), and has been featured by the CDC, the Associated Press, The Wall Street Journal, Forbes, and other media outlets. Follow him at @BenLocwin
For more background on the Genetic Literacy Project, read GLP on Wikipedia































