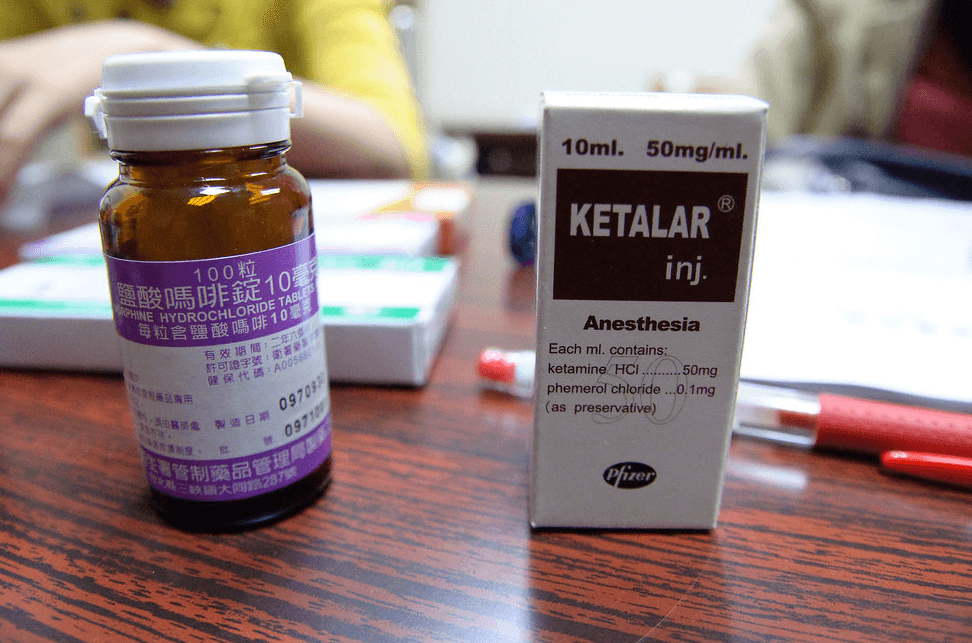
Ketamine is an FDA-approved anesthetic, a Schedule III drug recognized as having significant medical value. Since it’s FDA-approved, it can be used off-label. It also has psychedelic qualities, which have extended its use to non-anesthetic treatment. [1]
“When administered correctly and under the supervision of a professional, ketamine can be a life-changing treatment for major depression.”
Ketamine comes in two forms, both of which can be dangerous if misused. One, a racemic mixture (containing “R and S” molecules that are mirror images of each other), is an anesthetic. A second, Esketamine, having only the S form, is believed to induce an anti-depressant response in treatment-resistant depression and depression associated with suicidal ideation. It, too, is FDA-approved, but its use as an intranasal spray comes with boxed warnings and is strictly regulated.
Esketamine is to be used only in clinical settings with specified follow-up, including patients remaining in the facility for two hours after dosing. However, Esketamine is now being compounded, mixed with other agents to treat other psychiatric disorders. Compounded drugs are not FDA approved, causing the FDA to issue an alert over its use; both forms of ketamine pose dangers, and deaths have been associated with illegal use.
“There are also psychological risks. …either form of ketamine …has significant effects on cognition, …. [L]arge amounts of data suggest… that your ability to make rational, correct decisions is completely disrupted when you take ketamine as long as it’s in your system… about an hour and a half to two hours. It can also dramatically alter perceptions…. The physiological and psychological reasons are the main reason the FDA declared the drug safe only in a health care facility under supervision.”
– George Sanncora, MD PhD, Professor of Psychiatry, Yale Medical School
“Ketamine is a dissociative anesthetic that has gained popularity as a drug of abuse. Slang for experiences related to ketamine or effects of ketamine include “K-land,” baby food,” “Special K” and “God,” which refer to feelings of disconnection, surrealism, or memory gaps, caused by ketamine.”
Because ketamine is FDA-approved, it can be administered legally as lozenges, shots, or even infusions, conjuring vitamin or mineral infusions of health spas. Touting its off-label use to treat chronic pain and neuropathy (replacing opioid use) and medication-resistant mental health disorders including depression, PTSD, bipolar and mood disorders, “its purveyors, [claim its use is] supported by a growing body of research,” [2] notwithstanding its dangers and lack of regulation.
There is, however, at least one significant difference between the new ketamine clinics (the primary home of their off-label dispensation) and the centers set up for dispensing opioids. Opioids, especially the illegal variants, conjure the visuals associated with addiction, a perception fostering deterrence; not so ketamine, which has now found its way into the wellness and spa industry, even though the potential for abuse abounds, including diversion into the black market.
Imagine going for your ketamine fix to address those undiagnosed feelings of depression — or light out on a psychedelic experience. Walking into a spa-like atmosphere, one surreptitiously looks for a movie star or a mega-monied neighbor. The drug costs pennies to make. However, administered in these surrounds, it costs big bucks – between $4000 and 5000 for a course of treatment. The experience, patterned after the lucrative wellness industry worth an estimated $450 billion in the US alone, doesn’t come cheap.
While the patron’s “set” (or mindset) is important, the “setting” takes center stage. Specific visual and marketing cues predominate. Luxurious plant-clad walls dressed in blazing brights or soothing pastels– evoking a brilliant sunset in aubergines and azures, turquoise and coral — replete with silk flowers, furnished with zero-gravity chairs, weighted blankets, and eye-masks, generate an other-worldly experience. Tea, alkali water, health bars, and organic taro chips are provided with touches of whimsy, such as pencils and markers, all but obfuscating the medical significance of the “treatment.” The attention to aesthetics is so important that it generated its own term, “the rhetoric of space,” — when a physical environment communicates what it’s about and for whom.
Wellness capitalizes on transcendence, creating a “space” where a person can transform from their present state to a new, self-actualized state. The aesthetics of the space reinforce that message, confounding wellness with what is supposed to be a medical intervention. But experts say that “…psychedelics are not on par with a facial. And by putting such a treatment in a more entertaining or soothing setting, you run the risk of distorting the purpose and effect.”
These ketamine spas may include a handful of sessions and, of course, prescription and supervision by clinical staff, along, perhaps, with a post-experience talk called “integration,” where the client processes the experiences [3] but follow-up and attention to compliance go largely unregulated.
“Walk on in, get your vitamin infusion and walk out a new person. That’s now how psychedelics or any sort of mind-ordering substance works.”
As with other areas in the wellness industry, ketamine clinics have proliferated, increasing from 60 to 300 between 2015 and 2018, undoubtedly higher today. In some instances, the rush to gold has resulted in clinics overextending themselves, closing, and abruptly leaving patients in the lurch.
The health and wellness mismatch:
Till now, the wellness market has included nutritional supplements, yoga, crystals, Reiki, and green powders, but now, enhanced by ketamine – it lures those with money to spend seeking a new experience, enhanced wellness, or reprieve from psychological ailments. By associating ketamine with beauty and wellness, the serious effects and possible adverse reactions are air-brushed to the side. Informed consent doesn’t really figure.
“[w]hen you attach the clean design, the millennial wellness aesthetic, with something like ketamine, it imbues it with a sense of goodness and benignness that could be misleading.”
– Dr Coleen Derkatch, Professor of Rhetoric, Toronto Metropolitan University
Science, anyone?
As to the science behind the drug, its proof goes wanting. This week, the New England Journal of Medicine reported on the latest study of ketamine’s use for major depression. Results?
“Ketamine was non-inferior to ECT [electroconvulsive therapy] as therapy for treatment-resistant major depression without psychosis.”
This means ketamine isn’t any worse than the conventional treatment with ECT or any better. As for side effects, you trade the temporary muscle aches and cognitive symptoms of ECT for the dissociation of ketamine. After a month, any benefits of ketamine seem to evaporate, while the negatives (one suicide attempt and several episodes of suicidal ideation) remain.
European research, which included all types of depression (not just major depression), isn’t even as positive as the New England Journal of Medicine study.
The rebranding of ketamine as a wellness supplement might seem to complement existing mental health care. However, its use in this milieu can delegitimize research because many don’t take the wellness industry and its quick fixes seriously. It’s best to be aware that there are dangers from this medication, along with a lack of FDA attention which seems to vest, primarily, for now, only in guidance documents.
False advertising, anyone? Or maybe snake oil?
Notes:
[1] Interestingly, the newly proposed FDA draft on clinical experimentation with psychedelic drugs doesn’t name ketamine but focuses on Schedule I drugs, psyclobin (magic mushrooms), MDMA, and LSD. [2] With telehealth mushrooming during COVID, obtaining a prescription does not necessarily require a physical doctor visit. [3] Ketamine’s Woo-Woo Rebrand Harper’s BazaarBarbara Pfeffer Billauer, JD MA (Occ. Health) Ph.D. is Professor of Law and Bioethics in the International Program in Bioethics of the University of Porto and Research Professor of Scientific Statecraft at the Institute of World Politics in Washington DC.
A version of this article was posted at the American Council on Science and Health. Any reposting should credit both the GLP and the original article. Check out the American Council on Science and Health on Twitter @ACSHorg































