Avian influenza is surging again, but with an even deadlier twist: the scourge that has led to hundreds of millions of bird deaths since it was first documented in the 19th century may soon pose a COVID-like threat to humans.
The current iteration of bird flu, known as H5N1, has been escalating since the 1990s as the world poultry population surged exponentially to meet escalating food demand. It claimed its first known human victims in 1996-97, in China and Hong Kong, spread to Cambodia in 2003, and then reappeared with a vengeance a decade ago. According to the World Health Organization, it killed nearly 60% of the more than 800 people infected between 2003 and 2016. The majority of human H5N1 infections and deaths occurred in Egypt, Vietnam and Indonesia.
Despite these limited examples of person-to-person transmission, there are no known examples of widespread, sustained transmission among humans or any mammals for that matter. However, virus evolution called “antigenic shift” could give rise to the emergence of novel viral subtypes able to target mammals.
Recent isolated cases among humans have heightened concerns. At least six people were infected by H5N1 in Cambodia during 2023, four fatally. Last summer, at least two human fatalities in Poland were linked to a mystery outbreak among cats.
The deaths have public health officials worldwide on edge as fears mount that newly-mutated strains could lead to direct human-to-human transmission. Calls for more proactive global surveillance are escalating. Some scientists warn that a global health crisis that could rival the COVID-19 pandemic cannot be ruled out.
There is a promising solution that could protect birds and mammals, including humans, but, unfortunately, it is not being aggressively pursued. Gene-editing tools in development could likely contain H5N1 in birds by creating flu-resistant strains of chickens. A group of British scientists has used the CRISPR gene-editing system to tweak a specific chicken gene, ANP32A, that codes for a protein essential for the replication of the avian flu virus. The flu resistance traits were heritable and transmitted to offspring. But bureaucratic bungling, decades of misguided regulation, and doomsday claims by opponents of biotechnology innovation are blocking this promising solution.
Magnitude of the crisis as H5N1 spreads to mammals
There are currently no good ways to contain avian flu. Vaccinations are theoretically an option but are impractical; there are just too many birds. Each year in the U.S., approximately 8 billion chickens are slaughtered for their meat, and another 300 million are maintained for laying eggs.
Over the past 25 years, the US alone has recorded 72 million avian infections linked to H5N1 in commercial flocks, and wild birds, including gulls and terns, have also been affected, according to the US Department of Agriculture. According to the World Health Organization, more than 131 million domestic birds in 167 countries were lost due to infection or culling in affected farms and villages in 2022; and in 2023, another 14 countries reported outbreaks, mainly in the Americas. Some wild bird species are at high risk of disappearing altogether.

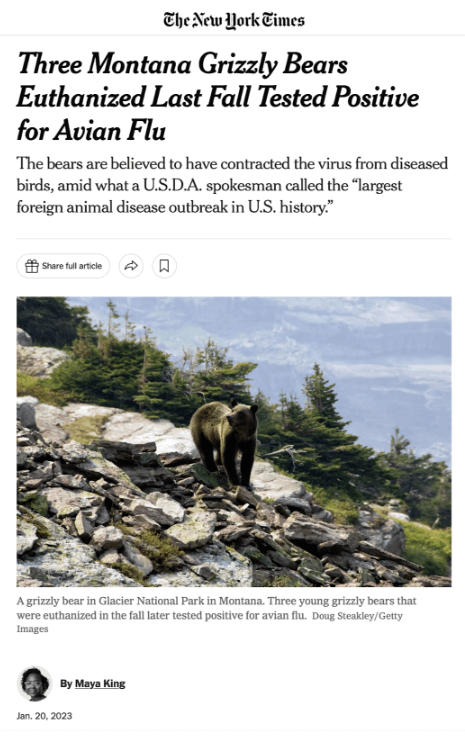
The deadliest recent twist is the spread of H5N1 to mammals. Brazil recently reported the deaths of more than 900 seals and sea lions, and thousands more were found dead last summer in Chile and Peru.
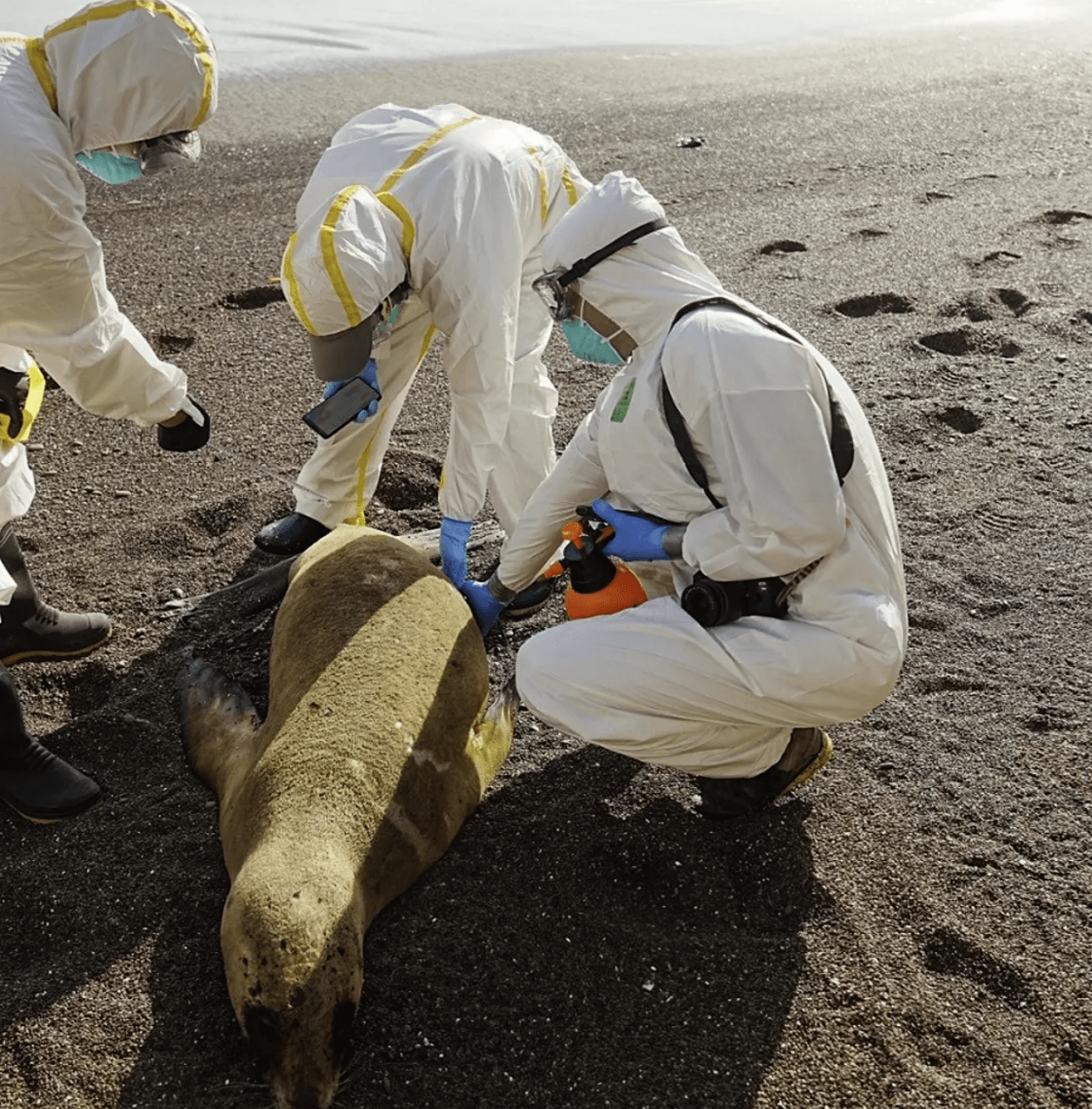
Washington State is on alert after dozens of seals showed up dead off the Olympic peninsula, alarming scientists. H5N1 has also infected large numbers of foxes, raccoons, skunks, grizzly bears and dolphins. Local authorities in all of these areas are scrambling to contain its spread, and warning humans not to touch the dead animals.
What can be done?
Many “zoonotic” viruses other than H5N1 spread readily in animals and can cross over to humans, although the latest variant is particularly lethal. New strains can arise that infect new hosts and evade immunity conferred by infection with their predecessors. Public health experts are concerned that that could happen with the H5N1 virus, and that the new viruses may be sufficiently different that most people will not have immunity to these “immune-escape” mutants.
There are two ways that new variants arise. “Antigenic drift” is caused by mutations in the virus’ RNA that change the virus’ surface proteins — hemagglutinin (HA) and neuraminidase (NA). Those mutations usually produce closely related viruses, so that antibodies elicited by exposure to one flu virus will likely recognize and neutralize to some degree the parental strain and other viruses that arose via antigenic drift.
Another, more drastic type of change, is called “antigenic shift,” which gives rise to new, significantly different HA and/or NA proteins in flu viruses that enable them to infect humans. This is more likely to occur when there is co-infection by different viruses — for example, human and avian flu viruses simultaneously infecting an animal host — giving rise to reassortment of viral RNAs and the emergence of a new hybrid virus containing parts of the genomes of two distinct viruses. The new viruses may be sufficiently novel that most mammals, including people, do not have immunity to them.
Dogs, cats, and wild birds, as well as some livestock such as pigs, ducks, and chickens, can harbor flu viruses. Many human flu pandemics have resulted when antigenic shifts created new hybrid viruses. Two of the most devastating flu pandemics, the Spanish flu (H1N1) and the Hong Kong flu (H3N2), resulted from such events.
What can be done?
Currently, there are no silver bullet solutions to containing the H5N1. Vaccinating chickens each year is impractical, given the numbers involved and the constant evolution of the virus. But gene-editing techniques offer hope. An article in Nature Communications recently described the creation of the world’s first flu-resistant chickens. Scientists at the University of Edinburgh, Imperial College London and the Pirbright Institute used CRISPR to modify ANP32A, the chicken gene that codes for a protein essential for the replication of the avian flu virus. The flu resistance traits were heritable and transmitted to offspring.
To further test the resistance to infection of the gene-edited birds, the researchers exposed them to a second, higher dose of the avian flu virus. The chickens again demonstrated suppression of viral infection, and further viral transmission to non-genome-edited birds with which they were in contact was significantly limited.
That is not the end of the story, however. Viruses are resilient, and the researchers found that in the gene-edited birds, in order to replicate, the virus adapted and enlisted the support of two related proteins, ANP32B and ANP32E. Additional editing to effectively remove from the genome the genes that code for those two proteins eliminated all viral growth in chicken cells. This suggests that editing the single gene the researchers first targeted (ANP32A) is not itself sufficient, so they intend to create new strains of chickens with mutations in all three genes.
If successful, the ability to confer resistance to avian flu could curtail infections and the culling of our poultry flocks, while at the same time substantially lowering the risk of transmission to wild bird populations — and humans. This would be of inestimable benefit to chicken farmers and consumers worldwide.
Kathleen L. Hefferon is an instructor in microbiology at Cornell University. Find her on X @KHefferon
Henry I. Miller, a physician and molecular biologist, is the Glenn Swogger Distinguished Fellow at the American Council on Science and Health. He was the founding director of the FDA’s Office of Biotechnology. Find Henry on X @HenryIMiller
Note: This is Part 1 of 2. The second part will discuss the regulatory obstacles to the commercialization of genetically engineered animals.