We’ve largely given up on the idea of a magical one-size-fits-all cure for the disease. Instead, cancer researchers are focused on finding ways to treat individual strains of the disease through personalized or precision medicine.
“Cancer therapy is becoming customized to each patient,” said Dr. Howard McLeod, medical director at the Moffitt Cancer Center’s DeBartolo Family Personalized Medicine Institute, in Tampa, Fla. “And beyond that, we’re even headed to a point when even the way that we monitor patients is individualized.”
Thus far, the idea of precision medicine has remained largely that – an idea, albeit one with a lot of promise.

A glimpse of the potential was demonstrated earlier this year, when researchers at the Icahn School of Medicine at Mount Sinai used fruit flies to develop a promising drug treatment for a patient with metastatic colorectal cancer. Essentially, they created more than 300,000 fruit fly avatars to stand in for the patient. According to New Scientist:
They then developed a robotic system to feed the flies and test different medicines on them. In this way, they screened 121 existing medicines – including both cancer drugs or treatments for other conditions – either singly or in combinations of up to three.
The approach led to a two-drug combo that showed promise for 11 months – significantly shrinking tumors – before new tumors developed that were resistant to the treatment.
While we are still a long way from seeing the routine use of fruit fly avatars in cancer treatment plans, the study raises hopes, said University of Colorado cancer researcher Tin Tin Su, who was not involved in the research, in an interview with The Scientist:
It is an exciting study. Nothing like this has been done before. Whether the approach will work, how applicable it is, that of course remains to be seen—it’s one patient. But you’ve got to start somewhere and this is an exciting start.
Learning from new information
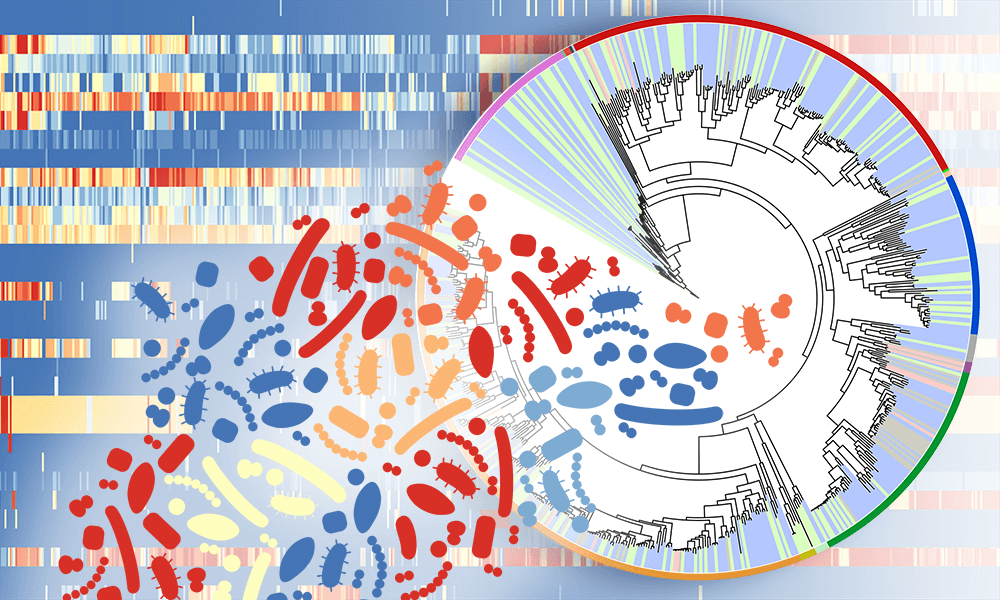
Much of the insight about the differences between what traditionally have been considered different cases of the same kind of cancer comes from what’s called multiomics – genomics, epignomics, proteomics, metabolomics and all the other “omics” from the molecular age.
In one sense, this perspective is simply the newest phase in a learning process that began centuries ago, when the word cancer (Latin for crab) was applied to any kind of growth or tumor that seemed to be from a patient’s own cells. The crab image fit with the anatomy of many solid malignant tumors (as opposed to blood cancers) that project claw-like extensions through healthy tissue.
But even by the early decades of the 20th century, when the principles of modern surgery had been established and when the science of microscopy pathology was coming to age, use of a single term, cancer, or the term malignant, was starting to make less sense. As an example, basal cell carcinoma (BCC) is a common form of skin cancer. It is called “malignant”, because it is not contained like tumors that are called “benign”. But while BCC can disfigure a person’s face horribly if it is ignored, it rarely ever metastasizes (spreads to distant points), so it is extremely unlikely to kill.
On the other hand, certain benign tumors — growths that are not cancer — can be deadly, based on their locations, or due to what hormones or other chemicals they secrete. Thus, for a long time, having a name encompassing all of the different diseases involving uncontrolled growth of a person’s own cells, has not made sense. Now, though, in the age of multiomics, the rationale for placing different cases of a cancer, for instance ductal carcinoma of the breast, into a common category, holds sway only to a certain extent. Said McLeod:
If you’re a surgeon or a radiation oncologist, anatomy still matters. But the move to personalized therapy applies to cases when there is a need for systemic treatment (medicines given throughout the body) or for any treatment that works by targeting particular molecules on and in cells.
Essentially, what this means is that personalized therapy comes into play, either when a cancer is metastatic, or when the cancer has been removed successfully, but is a type of cancer that carries a risk of appearing later at different sites if systemic therapy is not given. This means that say five or ten years from now, if a person develops BCC on the face, the treatment will be much the same surgery as it is today and won’t differ much between patients, but when it comes to various other internal cancer types there will be almost as many treatment approaches as patients.
Unfortunately, though, distinguishing one subtype of cancer from another is not as easy as distinguishing type 1 diabetes from a Strep throat. We have so much data coming in from cell surface proteins, DNA, RNA and other molecules of the cancer cells, and of the healthy cells that surround them. The formula for analyzing the body, either to work up a new cancer case, to screen for cancer as part of preventive health care, or to monitor for recurrence of cancer is getting to be so complex as to require artificial intelligence and machine learning algorithms.
Personalized cancer therapeutics
Big, disruptive changes in healthcare require industry to get involved, and this has started to happen in the case of personalized cancer therapy. A pioneer in this area is the company My Personal Therapeutics, founded and operated by biotechnology entrepreneur Laura Towart. Based in the UK, the company partnered with the Mount Sinai Center for Personalized Cancer Therapeutics, acquiring an exclusive license to commercialize the fruit fly avatar technology.
The process is not inexpensive. According to the company’s website, it costs $30,000 for its Personal Discovery Process – touted as a “massive clinical trial on a single patient.”:
We engineer the genetic complexity of each patient’s unique tumor network into an army of 400,000 fruit fly “avatars.” Using robotics, we evaluate up to 1,200 FDA approved drugs including non-cancer drugs, to identify drug combinations that significantly improve mortality in the individual’s avatar population.
This fruit fly avatar approach, isn’t the only technique under consideration for precision medicine.
DNA sequencing of tumors has been available for several years, offering doctors a way to take a closer look at a specific patient’s cancer, according to the National Cancer Institute:
In some cases, knowledge of the genetic alterations in your cancer can help determine a treatment plan. Some treatments—particularly, some targeted therapies—are effective only for people whose cancer cells have specific genetic alterations that cause the cells to grow out of control (these are sometimes called “driver” mutations).
There are, however, debates within the medical community about the value of tumor sequencing, with critics saying the promise is oversold – that only a small number of patients stand to benefit.
And as medical research is increasingly looking at the role of the microbiome in a wide range of human ailments, it should be no surprise that cancer is among them. A range of studies have raised hopes that altering our gut bacteria – through probiotics and transplants – could improve the way our bodies respond to various drugs. Jennifer Wargo is a professor of surgery and genomic medicine at the University of Texas who co-authored a review of microbiome science in February. In an interview with Smithsonian, she said:
We know that diet matters, but everyone wants to know what the secret sauce is to change the microbiome to respond better to cancer treatment. We simply don’t know that yet.
Perhaps the best known form of precision medicine is CAR T-cell therapy, in which a patient’s own immune cells are collected, genetically modified and re-infused into the patient. The therapy has been approved for “liquid cancers” non-Hodgkin lymphoma and a form of leukemia, with several other therapies in clinical trials.
The challenge for therapy is finding a way to make it work with solid tumors, according to an article in The Scientist. Among the problems is the fact that it is more difficult for T cells to infiltrate and remain in solid tumors. Nabil Ahmed, of the Baylor College of Medicine, told the magazine:
I don’t want to sound pessimistic, but solid tumors are not leukemia. [CAR Ts] need a lot of work before this [approach] can show efficacy.
David Warmflash is an astrobiologist, physician and science writer. BIO. Follow him on Twitter @CosmicEvolution